Editor’s note: “Our COVID-19 Fighters” is an occasional series highlighting the ways the CU Anschutz Medical Campus community is helping patients and the wider community in the fight against the pandemic. We welcome your story ideas; please share them here.
For Kristina Slunecka, it was the woman locked down in her assisted-living facility room, unable to leave the confines of her four walls even to go outside because of COVID-19.
For Desirae Martinez, it was the elderly man beginning their first call with, “I don’t have much to say,” and still chatting with his newfound friend an hour later.
The women were two of about 40 University of Colorado Anschutz Medical Campus students who reached out to the pandemic’s most vulnerable population as part of an innovative program launched by the Division of Geriatric Medicine and its UCHealth Seniors Clinic.
“We were worried about the patients not having access to care and having a lot of unmet needs,” said Sarah Tietz, a geriatric medicine fellow who created the program with her clinic colleagues. “Older adults have a lot of social isolation, and COVID-19 intensified that,” Tietz said.
“It ended up being a win-win for everyone involved.”
– Kristina Slunecka, CU Nursing student
When stay-at-home orders curbed non-emergent inpatient visits and isolated the nation’s older adults from loved ones, the Seniors Clinic staff responded with the creative initiative that served a dual purpose.
Answering a double call
Since late March, students have provided welfare checks via phone calls to the clinic’s 75-plus-year-old patients, who include aging veterans through a partnership with the Veterans Administration Medical Center on campus. Additionally, the program was approved to offer clinical hours for some students suddenly unable to meet their graduation requirements.
“It was a life-saver for me,” said Slunecka, a BS/DNP candidate in the CU College of Nursing who still needed 50 clinical hours when most rotation programs were ceased due to COVID-19. “It ended up being a win-win for everyone involved.”
Staff and students from CU Nursing, the CU School of Medicine and the Skaggs School of Pharmacy and Pharmaceutical Sciences joined the effort that has benefited students and the community’s older citizens during this time of crisis. “We’ve made more than 400 calls so far, and we will continue throughout the summer,” Tietz said.

From left to right: Dr. Janna Hardland, Dr. Sarah Tietz and Dr. Skotti Church, key organizers behind the innovative Division of Geriatric Medicine outreach program.
Martinez, a fourth-year medical student who connected with the man who went from little to say to an hour of storytelling, joined the effort in part to “remain grounded” in patient care during the COVID pandemic. “It was so enjoyable to be able to provide a listening ear, and it reminded me of the reason why I love geriatrics – connecting with the elderly population and making them feel valued.”
“Pretty overwhelmingly, the patients – even those who didn’t really have any needs – were grateful that somebody just cared enough to call,” Tietz said. Many patients opted for weekly calls, just wanting someone to talk to, she said.
Connecting the elderly
In addition to offering emotional and social support, students ensured patients had what they needed, from food and shelter to medications and caregivers. They helped older adults, many of whom didn’t know they could do telehealth visits, with setting up appointments and answered questions about medical and prescription concerns.
“I spoke with a daughter about a side effect of a medication her mother was having and then realized she wasn’t taking appropriate doses,” said Susan Hines, a student in CU Nursing’s Adult Gerontology Nurse Practitioner program. “I was able to get that information to the provider.”
When they learned from their peers doing the calls that many patients didn’t realize they could have prescriptions mailed or delivered, pharmacy students compiled a list of local pharmacies and their COVID-related policies.
“Most pharmacies have been offering free delivery and mail service,” said Scott Pearson, assistant professor of pharmacy who organized and oversaw the pharmacy students. “So, the pharmacy students provided that list as a resource for the other students,” Pearson said. “I think that was certainly helpful for a lot of patients.”
Teamwork across disciplines
Divided into teams with at least one pharmacy, nursing and medical student on each, the groups met weekly, discussing that week’s patients as well as case studies provided by the Division of Geriatrics. Case studies focused on geriatric issues, from osteoporosis and dementia to diabetes and falls, and were added to enrich the learning experience for students.
“We pre-rounded on patients,” Holly Truong, a fourth-year pharmacy student said of discussing patient cases each week. “I would look at their medications and see if there was anything I needed to let the other students know before their calls,” Truong said.
Many participants, Slunecka included, found the multidisciplinary aspect highly valuable. “I feel like that’s a really useful tool in my current job (as a patient navigator) and even moving forward in my nurse practitioner career,” she said.
“Coordinating with different disciplines and being aware of their different roles within the team is crucial. Everybody brings something to the table,” Slunecka said. “It was really nice having the pharmacy students reviewing these cases to help guide the care.”
Caring for the elderly
For some students, including Truong, the program attracted them toward geriatric care. “It definitely strengthened my desire to want to help the older patients and maybe specialize in geriatrics after I graduate,” she said.
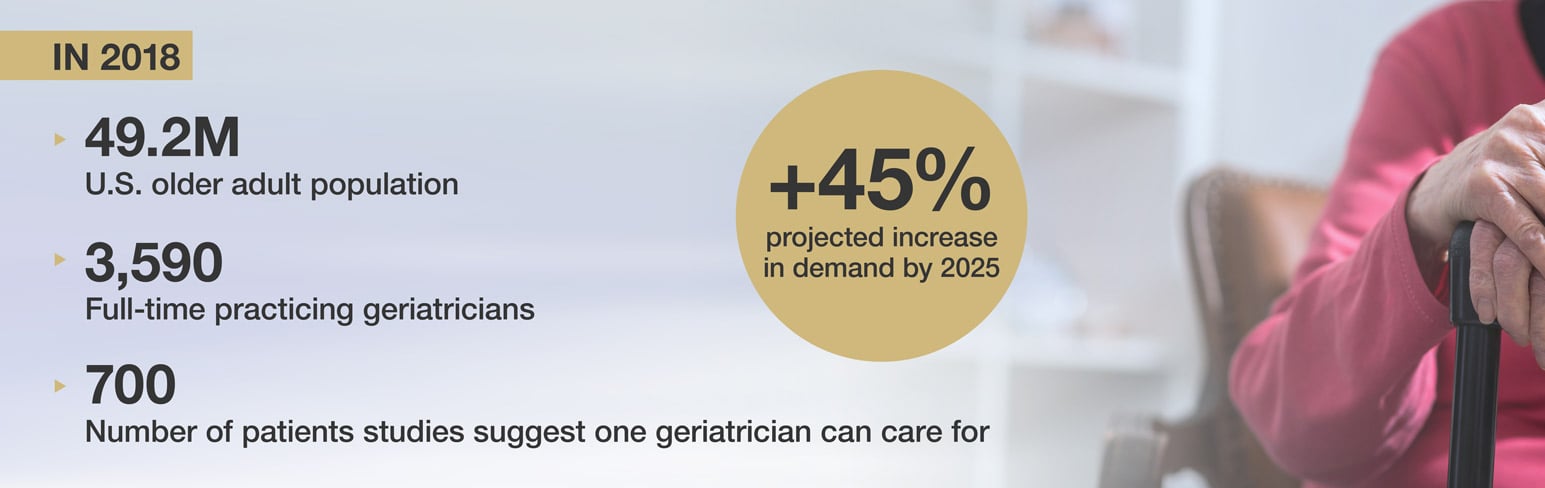
With a dramatic shortage of geriatric specialists and an older adult population expected to more than double in the next 20 years, that’s good news for the field, Tietz said.
“Really, students going into most fields are going to deal with older adults,” she said. “So, giving them experience with older patients and the medical challenges that come with them is important for all.”
Photo at top from left to right: Students Holly Truong, Desirae Martinez, Susan Hines, Karima Hamamsy and Hailee Griffin.