Editor’s note: “Our COVID-19 Fighters” is an occasional series highlighting the ways the CU Anschutz Medical Campus community is helping patients and the wider community in the fight against the pandemic. We welcome your story ideas; please share them here.
Haley Cehura remembers being nervous entering her first COVID-19 patient’s room. During the procedure, which took three hours, she began feeling a little weak. When she finally left the room, her eyes welled with tears.
“Why am I so worried?” she wondered. “This is what I do.”
As a veteran critical care nurse, Cehura had often thought to herself while caring for patients: “What if this were my family member? What if this were me?” But this time was different.
“It just became so real that it really could be me or my family,” said Cehura, BSN, RN, CCRN, a University of Colorado College of Nursing alumna and charge nurse in the Neurosurgical Intensive Care Unit at UCHealth University of Colorado Hospital.
“It was scary. I thought: What do I do when I go home tonight?” she said, worried about possibly spreading the virus to her husband. “And: Are these patients going to survive?”
But within days, because of her hospital’s rapid response to the unknown illness and the skill, commitment and camaraderie of her medical colleagues, Cehura said a widespread mentality took over: We’ve got this.
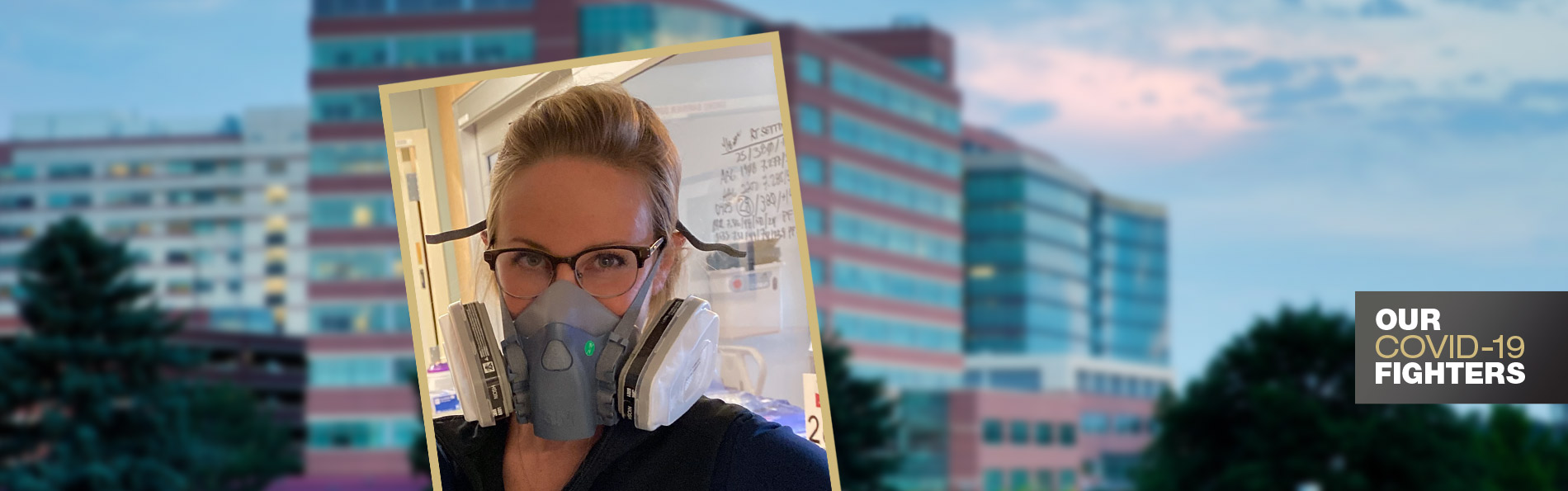
Haley Cehura, a critical care nurse at UCHealth University of Colorado Hospital.
Cehura shared more about the struggles and successes of being a nurse during the coronavirus pandemic in honor of National Nurses Week (May 6 through May 12):
What is it like being a nurse during this pandemic?
I would say it’s been a surreal experience. Within a matter of days, it just began evolving and changing, and I think all of us started to realize: We really don’t know what this is. It started to become a little bit scary. But as the days went on, and we realized that the hospital was there for us and had plans in place before we even knew about them, it just started to become: All right, we’re doing this, and we can do this.
How would you describe COVID-19 as a medical challenge?
We deal with respiratory illnesses all the time, but this one was just different. Doctors (many of them joining the patient-treatment effort from different specialty areas) are tirelessly researching. And the nurses, we’re also looking to our educator to provide us with resources, and we’re studying on our days off. How do we treat this disease? What is different about it?
Also, what do we already know? How do we treat respiratory illness and ARDS (acute respiratory distress syndrome) already? So, we are treating it how we know to treat a respiratory disease, but with a twist. There are new medications. There are new things that we are doing. We’re all just working together to treat it, and we’re doing a great job. We’ve seen so many success stories.
How fearful are you for your own health and your own family?
The first night, I slept in the guest bedroom, because I was worried about my husband. But we are realizing this isn’t going away for me. I live with my husband, and I have to risk his health, and that’s something that is just a reality for us.
Another question is: How do I decide when I can see the rest of my family? I haven’t seen my niece or my nephews. I haven’t seen my mom or my dad or my siblings or my friends. What happens if a family member gets sick, and you were around them? Is that your fault? I’m on the Mobile Stroke Treatment Unit as well, so I also go out in the community with EMTs and firefighters, and they’re all concerned. It’s one of those things: What do we do with this? What do we do moving forward? Because this could be another year, another two years. Especially when the community goes back to a little bit more of a normalcy, we’re going to continue to see these patients.
Haley Cehura focuses on time with her husband and hobbies in practicing self-care.
How do you deal with the fear of the unknowns?
Counseling through my coworkers has been a huge thing. Some of us charge nurses, every night after our shift, would get on a Zoom call and just talk for like two hours and decompress. We were joking that we’re like the COVID Wives Club, because we need each other to lean on and support each other.
And then also not talking about COVID, telling people I need a break from it. My family knows when I need a distraction and just need that time away from it. My husband’s really good at that. On our days off, we’ll garden, or pick up the yard, or work in the garage on our dirt bikes. We’re getting those ready and waiting for the trails to open. I’ve been running. My mom and my sister and I are doing half-marathon training. And then some days are just couch days and maybe a glass of wine. It’s just been cool, because everyone at the hospital is like: We’re all in it together. We are a community. You don’t really feel alone.
What are some of the hardest aspects for your patients and their families?
That was one of the craziest parts. I never thought in my career that a visitor wasn’t going to be allowed in a hospital, that patients weren’t going to be able to be with family members during the hardest times of their lives. I truly never imagined that ever happening, and it’s hard for them (especially when a ventilator becomes necessary). They are having to get on an iPad call with the nurse and tell their family members: OK, we are doing this now, and it’s scary. The patients are scared, and I know the families are scared. I can’t imagine.
So, we are taking that role as the “family member.” Most nurses are staying in their patients’ rooms for well beyond what they normally would just to have those interactions on that iPad. And families are coming to the windows to be able to see their loved ones in the rooms, and we are making those efforts. We’ve been making that a priority in patient care.
Pets and exercise help Haley Cehura forget about COVID-19 for a bit.
Is there anything else about working for UCHealth University of Colorado Hospital that stands out?
A lot of what they have done has been amazing. I think the biggest thing that was helpful is how prepared they’ve been from the beginning. They didn’t hesitate. We were canceling these elective surgeries. We were clearing out ICUs. In the beginning, I was scared: Are we going to have room? Are we going to have supplies? Are we going to have ventilators? But it felt like every time I was worried, they were a step ahead. They already had a plan in place. They had resources out for us. We got tons of support from them, even food. It sounds silly, but they wanted to make sure that we were fed and mentally well. They have people to talk to us if we need, and they are making sure we practice self-care.
What else would you like the public to know?
We’re feeling the same way they are. This is something that no one has dealt with. And they are also heroes. They are the ones who are having to stay at home, and I feel horrible for the people who are losing their jobs and possibly not being able to pay their rent and mortgage. That’s just as heroic as us on the front lines. We are putting ourselves at risk and taking care of these patients, but we still get paid. We appreciate them supporting us and supporting the community.