What is rheumatoid arthritis and some of the first symptoms of the disorder?
It’s an autoimmune disease in which a person’s own immune system gets confused and starts to attack them. The immune system does damage to the joints. Early signs and symptoms include joint pain and swelling. Commonly affected joints are in your hands, wrists, elbows, feet and ankles. If a swollen joint also has stiffness in the morning that lasts more than an hour, that is a huge red flag.
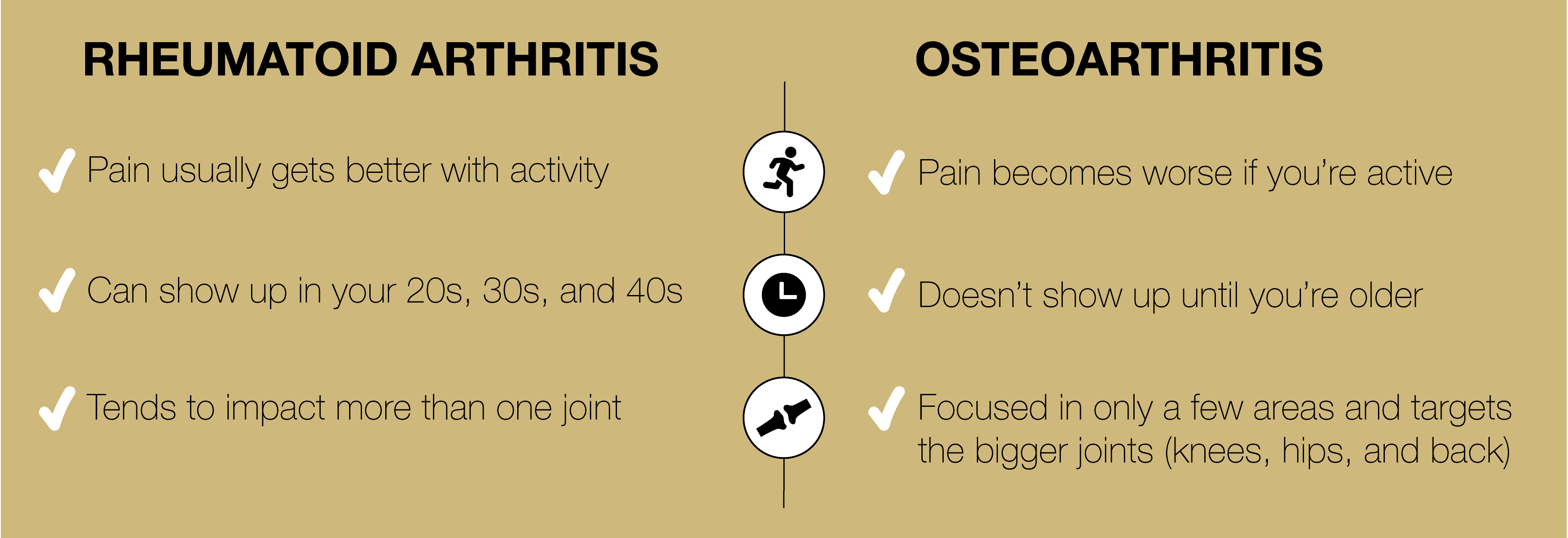
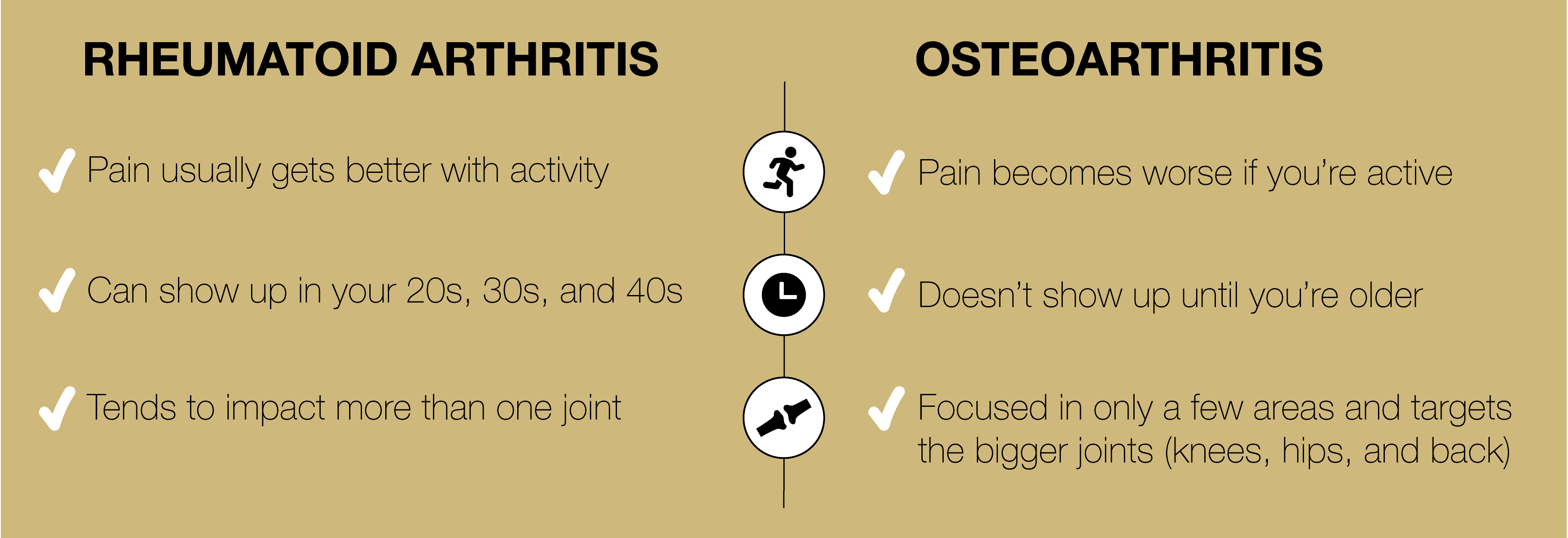
What makes RA different from osteoarthritis?
Osteoarthritis is what we call “wear and tear” arthritis that happens after years of use – a degenerative condition. With RA, your pain usually gets better with activity. In contrast, if you have osteoarthritis, your pain usually becomes worse if you’re active. RA can show up in your 20s, 30s and 40s, whereas osteoarthritis usually doesn’t show up until you’re older. RA also tends to impact more than one joint, whereas osteoarthritis is usually focused in only a few areas and targets the bigger joints (knees, hips and back).
What triggers RA, and are some people higher risk than others?
We think it’s a combination of underlying genetics and environmental triggers, so it’s usually not one single thing. One of the things we study is mucosal sites (gums, lungs, GI tract, genital tract) where the immune system interacts with the environment. Your immune system reacts to lots of things like a virus, infection or cigarette smoke by increasing inflammation to attack the foreign “intruder.” But in people with RA, we think the system overacts and doesn’t stop once the “intruder” is gone.
Many think this is a disorder that shows up when you’re older, but it can emerge at any age. Can you tell me a little more about that and the risk of not treating it early?
"It's true that the average age when people are diagnosed with RA is in the 50s, but RA can definitely begin for many people at younger ages. When that happens, we often see younger people, especially those who are physically active, who often initially write off the symptoms as soreness and joint pain related to their fitness activities. It’s also common in postpartum women, who rationalize their fatigue and aches. New mothers are tired from not sleeping, so they ignore the fatigue. Their wrist hurts, but they think it’s related to holding their baby, so it can take a while for someone to realize something else is going on.
The danger of letting it go untreated is that it could lead to damage of the joints and bones causing deformation and possibly disabling the use of the joint altogether. If that level of damage occurs, that’s something we can’t fix right now with currently available therapies. Studies are clear that if you get onto appropriate treatment earlier, like within a few months of symptoms starting, the long-term outcomes are significantly better, and joint damage can be avoided.
Can you talk about the blood test that can help diagnose RA?
The blood test is called anti-CCP, is very helpful and something you can easily ask your primary care physician to run. It’s important to note that 30% of the people who have RA will test negative for the antibodies, so it’s not fail proof. Also, the blood test being positive doesn’t always mean you have RA. It can be positive in some people who don’t have symptoms, and in those cases, the blood test is a good predictor that you are likely to develop RA in the next few years, which could give you a jump start on treatment. It’s never a bad idea to get the test run just in case, and if it is positive, you should definitely see a rheumatologist to find out if you have RA or if you are at high risk of developing RA in the future.
Let's discuss the treatment plan. I've discovered it's a long road with a lot of experimenting and something that changes the rest of your life.
Fortunately, there are a lot more treatments available than there were two decades ago. Patients usually start out with less potent and more cost-effective oral treatments before moving onto biologics if those don’t work. It’s a stepwise approach to therapy and required by most insurance companies. Biologics are great because they target certain inflammation pathways and have proven extremely effective for many patients. However, you may have to try several medications over the course of months to see which one works for you, which is a major downside to our current treatment approaches. Also, since your immune system is lower on these treatments, you’re going to have to get more vaccines to help protect it. And you’ll be going in for regular blood tests so that your rheumatologist can keep on top of any abnormal results.
Are there any new treatments for RA on the horizon that seem promising?
New treatments for rheumatoid arthritis (RA) are being developed and tested. One exciting option is CAR-T therapy. This therapy takes a person’s immune cells, changes them to attack harmful cells causing inflammation, and then puts them back into the body to help reduce RA symptoms. The Rheumatology Division at the University of Colorado Anschutz Medical Campus is testing this in clinical trials, including one for hard-to-treat RA. These trials are helping scientists see how well the treatment works. Another focus is finding ways to prevent RA before it even starts, especially for people at high risk. If these treatments succeed, they could help millions of people avoid RA pain and damage.
For younger people diagnosed with RA, understanding the impact it's going to have on the rest of their lives can be overwhelming and a bit frightening. What would you tell us as we navigate these new waters?
There are helpful online tools through the Arthritis Foundation (www.arthritis.org) that contain information, links to support groups and education. Connect with others, use support groups and patient-directed education. You are not in this alone.