The emergency room was overflowing with sick patients. The graduate nursing student had 15 minutes to figure out what was wrong with the deathly ill woman, consult with his colleagues, and get her help. With the clock ticking, he asked questions about her medical history and examined her. Was she suffering from sepsis, bacterial meningitis, gastrointestinal bleeding, or a number of other life-threatening conditions? Minutes later, everything froze. Time was up. The patient and emergency room vanished as the program shut down.
Advanced practice registered nurse students at the University of Colorado College of Nursing immersed themselves into virtual medical emergencies to simulate what they could not initially get in the spring of 2020– real world clinical training and experience. The pandemic restricted many of them from practicing in actual clinics with real patients because of limited physical clinical workspace, and less preceptor availability. Yet, the students were still required to earn clinical hours for indirect patient care to graduate. That prompted the faculty to get creative.
As an alternative to traditional clinical experiences, CU Nursing faculty Angela D. Pal, PhD, ACNP-BC, CHSE; Fara Bowler, DNP, APRN, CHSE; Mary Beth Flynn Makic, PHD, CCNS; and Krista R. Estes, DNP, FNP-C introduced an established, computer-based virtual simulation for grad students. In an article just released, the faculty says the virtual simulation training kept the students engaged and taught them how to handle emergency situations almost as well as the real thing.
According to the faculty, while research is limited, a systematic review found this mode of education improved nursing student skill-base, cognitive and affective knowledge. It provides an opportunity to improve patient safety, work effectively as an interprofessional team, develop communication skills, and critically think. Simulation facilitates autonomous learning because the student can repeat the scenario for a more deliberate, focused experience.
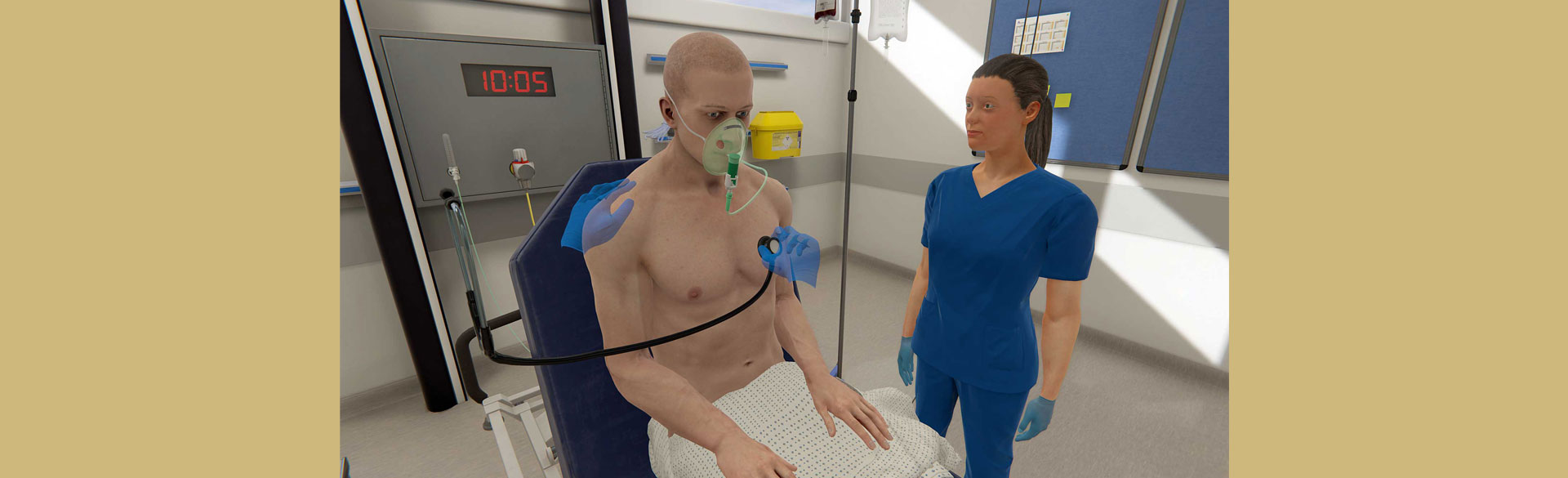
Faculty used the Oxford Medical Simulation (OMS) platform, which follows best practices in simulations. Students had 15 minutes to assess, diagnose, offer empathy, collaborate with other providers, analyze the results and the patients’ medical records, and treat the patient.
OMS uses artificial intelligence to adapt to the virtual patients’ conversations, behavior and physiologic responses to the students’ interventions and questions. After the simulation, students completed a worksheet about the scenario and received feedback about their encounter.
During the year-long program evaluation, 144 graduate students volunteered to participate in the virtual clinical education. According to a survey, 86% of the students said it accurately reflected clinical practice.
“I found this to be of value to our program… This simulation includes all the components to complete a full history and physical, order labs, diagnostics and treat the patient effectively in a given time,” said one student participant.
With the successful simulation, faculty plan to continue using virtual reality to enhance student learning and clinical experience.