When a patient experiences chronic eye pain, there could be myriad reasons causing it, so figuring out the root of the problem can be like putting together a puzzle, says Cara Capitena Young, MD, associate professor of ophthalmology and medical director of the Sue Anschutz-Rodgers Eye Center operating room.
In two recent separate cases, Capitena Young and fellow ophthalmologists at the University of Colorado School of Medicine were able to trace patients’ chronic eye pain to stents implanted in the eye to reduce intraocular eye pressure (IOP). Through removal, the team of eye experts were able to continue to treat the patients’ glaucoma and successfully remove the devices to alleviate the pain.
Luckily, these cases of chronic pain after glaucoma stent placement are not common, Capitena Young says. However, removing the tiny stents, which are typically about the length of a pencil eraser, can be complex.
“Because these instances are so rare, there is a lot to consider about the case and what it means for the patient,” Capitena Young says. “As a glaucoma specialist, you’re equipped to handle both low pressure and high pressure, which can happen with most glaucoma surgeries, but in these cases with a rare and complex removal, you must do a lot of prep work because there are more unknowns.”
In addition to the risks that could follow the surgery, Capitena Young also had to prepare for an operation neither she nor many ophthalmologists around the country have completed.
In one of the two cases, she removed a CyPass microstent, a minimally invasive glaucoma surgery (MIGS) device that was recalled from the market in 2018 following safety concerns. The patient, who was referred to the Sue Anschutz-Rodgers Eye Center after having the initial surgery elsewhere, experienced chronic eye pain for years following the device’s implantation in 2017. Capitena Young only knew of a few surgeons in the U.S. who had performed this specific MIGS removal surgery previously. She consulted with them, as well as the glaucoma team at the Sue Anschutz-Rodgers Eye Center, then reviewed their techniques to tailor to her own case.
In the end, the removal was successful.
“The day following the surgery, I was expecting the patient to have pain and discomfort from the surgery itself, but when I walked in the room, the first thing the patient did was stand up and hug me," Capitena Young recalls. "They remarked the pain they’d been experiencing for years was gone. It was pretty startling to me that this removal had such an enormous impact on their quality of life so suddenly."
Leveraging an expert team
These cases of atypical eye pain following stent surgeries are a reminder, Capitena Young says, that patients and ophthalmologists alike can benefit from an environment where there are clinicians with different specialties, experiences, and a plethora of resources.
Physicians across the CU Department of Ophthalmology consulted with the patient who ultimately had the CyPass removal to rule out other potential culprits, such as dry eye issues, which can cause pain and discomfort similar to what this patient was describing, and thyroid eye disease.
When Capitena Young scrubbed in to perform the CyPass device removal, she was assisted by Mina Pantcheva, MD, associate professor of ophthalmology. A handful of other CU ophthalmology faculty members and fellows were also there to offer suggestions on safely removing the device and limiting damage to the eye.
“We have a wide breadth of knowledge and experience at our fingertips here, and everybody is always willing and ready to help,” Capitena Young says.
Pantcheva says when Capitena Young pulled out the device, which took about an hour, she knew almost immediately it was likely the culprit for the pain.
“I had the most expert assistant in the world,” Capitena Young says of Pantcheva. “When I felt like I needed two hands, she was already doing what I was about to ask for. It’s like our brains were linked during that case.”
‘No textbook definition’
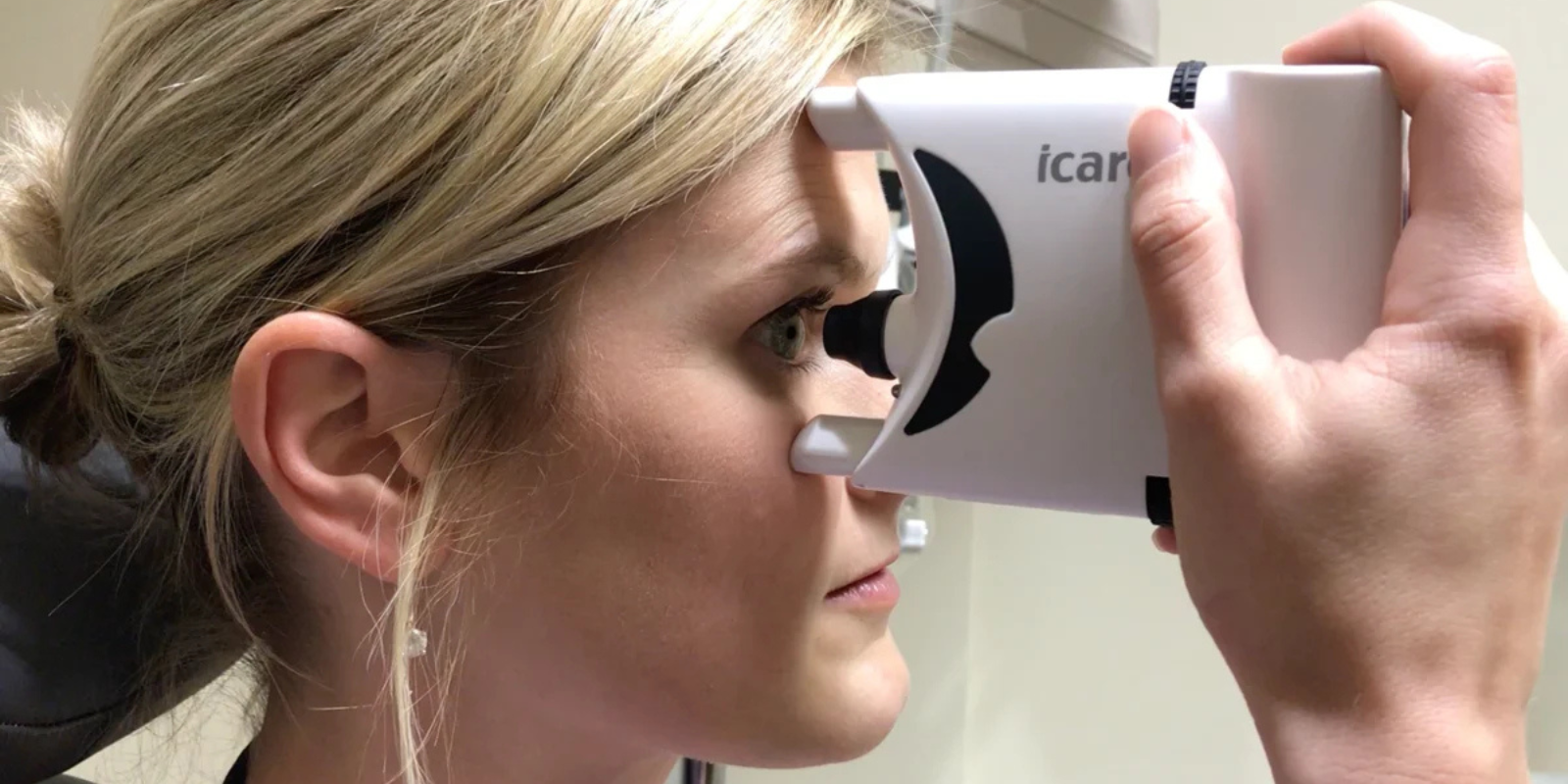
Thousands of patients receive stents for glaucoma management each year, and only a small percentage experience chronic, atypical pain afterward. Still, if something feels off, Capitena Young and Pantcheva say it’s worth investigating.
“If you're not getting answers or finding relief, it's never a bad idea to get a second or a third opinion, because each physician has different experiences, and no patient perfectly fits a textbook definition,” Capitena Young says. “Each patient is unique, and different factors play a role. If your pain onset with a certain event, like a surgery, and didn't resolve when that event resolved or healed, that’s something to be wary of.”
Pantcheva echoes those sentiments and adds that the power of teamwork seems to be an important factor in a patient’s success.
“In future cases similar to these, I would recommend having more than one surgeon involved in retrieving a stent,” she says. “You’re assured that you have at least two brains and four hands working on the problem.”


.png)