Generating retinas from stem cells and transplant technologies to restore human sight felt like just a dream for Valeria Canto-Soler, PhD, associate professor of ophthalmology in the University of Colorado School of Medicine. When she joined the CU Department of Ophthalmology faculty in 2017, she signed on as the inaugural director of CellSight, the department’s ocular stem cell and regeneration research program, setting benchmarks 15 years in the future.
Five years since CellSight launched, the program has revolutionized ocular stem cell-based technologies, not only exceeding its own goals, but also becoming established as a global leader in the fight to prevent blindness in diseases such as age-related macular degeneration (AMD).
“Currently, the main focus of CellSight is to develop a stem cell-based therapeutic approach to dry AMD, which affects the retina and leads to irreversible vision loss,” says Canto-Soler, who is also the Doni Solich Family Chair in Ocular Stem Cell Research. “We are using our stem cell technology to grow miniature human retinas in culture as a product to replace the retinal cells that are lost during AMD.”
“The dream was to develop a retinal transplant containing photoreceptors and retinal pigment epithelium cells and start transplanting it in animal models,” she continues. “We thought we might be ready to start thinking about the transplant process after five years. Those five years have already passed, and that dream is already underway with very promising, preliminary results,” she continues.
The building blocks to begin research
Top-notch research requires state-of-the-art facilities. Construction of the CellSight facility laid the foundation for the quick success of the program, taking nearly all of 2017 to build. Located at the CU Anschutz Medical Campus, the CellSight laboratories required extensive collaboration between engineering and architectural teams to design and build a facility capable of meeting demanding environmental conditions, complex workflows, long-term cell culturing, and strict anti-contamination protocols.
“We were able to customize a state-of-the-art facility that is unique, holding up to 60 cell culture incubators,” explains Natalia Vergara, PhD, director of the Ocular Development and Translational Technologies Laboratory within CellSight. “Everything needed to be built with the idea of avoiding contamination. Our cultures, which mimic human retinal development both in space and time, can take up to six months to reach a mature state needed for our research applications.”
Using cells derived from the skin, blood or even urine of patients, CellSight researchers needed an environment conducive to transforming these cells into pluripotent stem cells, and then ultimately into miniature retinas grown in petri dishes.
The delicate process of real-time human retinal development meant the facility required culturing and quarantine spaces with appropriate lighting and air flow, automatic opening doors, experimental rooms, a transgenic suite, and ample temperature-controlled storage.
“We also built a facility that would accommodate growth,” Vergara says. “Starting with maybe five or six people, we envisioned expanding our team to over 50 people and having enough room to do so. We are already filling those rooms.”
Currently comprising five complementary research groups led by Canto-Soler, Vergara, Joseph Brzezinski, PhD, Miguel Flores-Bellver, PhD, and Marc Mathias, MD, the formation of the CellSight team was crucial to building a strong foundation.
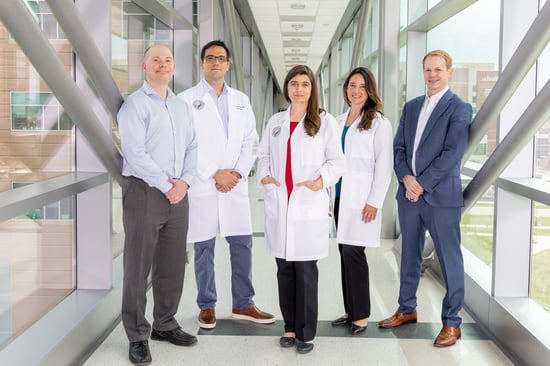 CellSight is led by Joseph Brzezinski, PhD, Miguel Flores-Bellver, PhD,
CellSight is led by Joseph Brzezinski, PhD, Miguel Flores-Bellver, PhD,
Valeria Canto-Soler, PhD, Natalia Vergara, PhD, and Marc Mathias, MD.
“Dr. Canto-Soler was the ideal candidate we sought to lead our efforts to develop an ocular stem cell program in the Department of Ophthalmology and in collaboration with the Gates Center,” says J. Mark Petrash, PhD, professor and vice chair for research in ophthalmology at the CU School of Medicine, and associate director of the Gates Center for Regenerative Medicine. “Her commitment to build collaborations needed to succeed in transformational research reflected the guiding principle of Charles C. Gates, who famously said, ‘Nobody does their best work alone.’”
The founding team included 6 members, most of which uprooted their families to move to Denver and create CellSight. The team now involves 24 internationally recruited staff and trainee members.
“The team that we dreamt about years ago was nothing but a profile I wrote out on a piece of paper,” Canto-Soler recalls. “That team exists today and surpasses my own expectations.”
Overcoming barriers to develop groundbreaking retinal technology
Because such retinal transplants have never been tried before, the CellSight team has developed everything from scratch over the past five years.
“The nature of the transplant that we are developing is unique, so we had to go from zero,” Canto-Soler, who leads the 3DRet Laboratory, says. “You have to solve all the problems of a new technology that no one else has tried to develop before. There were no surgical instruments to manipulate and deliver this type of transplant. We had to design the right tools to use and adapt the surgical procedures to suit the clinical product that we are working toward.”
A significant CellSight innovation has been the use of noninvasive imaging technology to assess the functionality of the retinal tissue. Collaborating with NanoScope Technologies, LLC, a company focused on the development of biomedical devices for diagnostic and therapeutic applications, the CellSight team established a noninvasive assessment that allows functional evaluation of the retinal transplants before and after implantation – not only in a research setting, but one that could be translated into clinical care. Together, they also developed a model using a laser to mimic AMD to more accurately test their retinal transplant approach.
“In macular degeneration, you have retinal pigment epithelium (RPE) behind the retina which becomes damaged, and you have photoreceptor cells that are juxtaposed to it that are injured or lost. But initially, the rest of the retina is not degenerated,” Vergara explains. “In collaboration with NanoScope, we were able to develop a technology to specifically injure the RPE and the photoreceptor cells in animal models, leaving the rest of the retina uncompromised, creating a model that is better suited to our purpose.”
With the new model, CellSight performs surgeries by inserting this transplant in the area of the retina that has been damaged by a laser, using surgical instrumentation developed by a team of retinal surgeons led by Marc Mathias, MD, associate professor of ophthalmology at the CU School of Medicine. The transplant is then tracked to assess whether it maintains its structure and whether it remains functional.
“The preliminary results are extremely promising with evidence of electrophysiological activity of the transplanted complex,” says Naresh Mandava, MD, chair of the Sue Anschutz-Rodgers Eye Center. “We still do not know if there is active integration or communication of these transplanted cells to the remaining retina, as well as downstream through the optic nerve into the brain, but we have a great deal of excitement knowing that the cells are surviving and have retinal function.”
Groundbreaking research and innovation like this has earned the CellSight team awards from the National Eye Institute and one granted patent, with five more patent filings under review.
The promise of patient care
In addition to collaborations with clinical development companies, the program has partnered with other academic institutions, as well as multidisciplinary teams across the CU Anschutz Medical Campus. From basic researchers to clinicians, CellSight prides itself on the synergy they’ve created to improve patient outcomes.
“Coming from different labs, universities, and organizations, our environment is unique – not only by how hard everyone works, but how easily we are able to address problems since we all come from various areas of expertise,” says Flores-Bellver, who leads CellSight’s ExoSight Lab. “Everyone brings something special, and we know we need that to move forward. I haven’t seen this level of collaboration before in other places.”
As the program’s goals continue to advance, researchers ultimately hope to bring their discoveries into clinical trials and deliver newfound sight solutions for people with degenerative eye diseases.
“This is hard work. We are committed to finding a cure for blindness, and we’re aiming to do it in a way that has not been done before,” Canto-Soler says. “At CellSight, we are dreamers and believers, and without the support from our donors and friends, CellSight would still be just a dream.”
“We cannot promise that we will cure blindness," she continues. "But in honor of Doni Solich's wish for us to carry out research on macular regeneration, we believe if there is a way, we can do it.”








.png)