Researchers in the Division of Ophthalmic Epidemiology in the University of Colorado Department of Ophthalmology have confirmed an association between vision loss from advanced age-related macular degeneration (AMD) with depression, following a study of patient data collected over seven years. This finding will help bring visibility into the impact of the disease, which is a leading cause of vision loss for older adults.
“In this study we show that the patients with geographic atrophy (GA) AMD who have no available treatment have lower mean mental health scores than patients with neovascular (NV) AMD, which can be treated,” says Cheryl Fonteh, MD, MS, CU School of Medicine resident and lead author of the study published in a recent issue of the BMC Ophthalmology journal.
AMD doesn’t cause complete blindness, but those in advanced stages of the disease can lose their central vision, making it harder to see faces, read, drive, and perform activities of daily living. Not everyone with AMD experiences progression to the advanced stage, and the medical community classifies it according to stages – early, intermediate, and advanced, and further classifies the advanced stage into two subgroups – NV and GA.
 Normal vision (left) compared with simulated image of vision loss occurring with age-related macular degeneration (right). Images courtesy of the National Eye Institute.
Normal vision (left) compared with simulated image of vision loss occurring with age-related macular degeneration (right). Images courtesy of the National Eye Institute.
Those in the advanced stages of the condition can be at higher risk for depression, and researchers at the Sue Anschutz-Rodgers Eye Center set out to better understand the disease trajectory by studying 875 AMD patients enrolled since 2014 in the University of Colorado AMD registry. In 2021, the AMD research group received $1.6 million in funding from the National Institutes of Health (NIH) to support select studies from this registry.
The registry contains patient information, including eye images, specimens to track biomarkers in the blood such as inflammation levels, and results from an NIH questionnaire assessing visual functioning that includes a section on mental health.
By categorizing subgroups of AMD, CU researchers found a very strong association between mental health and vision loss in later stages of the disease.
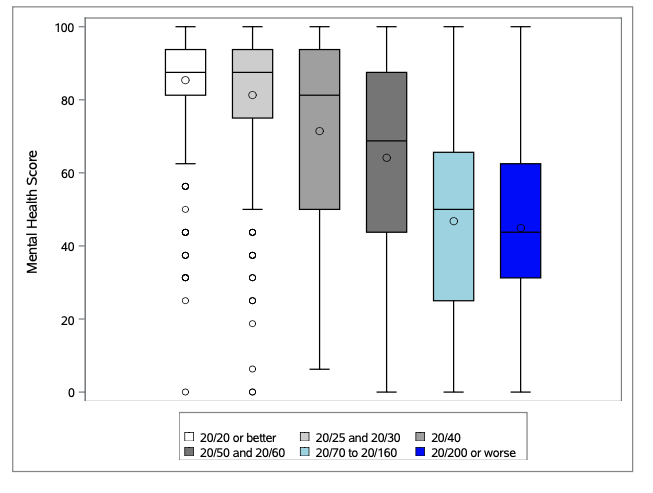 CU researchers found mental health scores declined as vision declined in patients with adult-related macular degeneration (AMD).
CU researchers found mental health scores declined as vision declined in patients with adult-related macular degeneration (AMD).
“The association is kind of obvious,” says Jennifer Patnaik, PhD, MHS, assistant professor of ophthalmology. “When vision declines, a person can lose the ability to perform some independent activities such as driving and reading, and that has a big impact on a person’s mental health.”
By better understanding the disease trajectory in patients with the various stages of AMD, CU researchers hope to create an AMD progression risk score that will improve the timing of therapeutic interventions, mental health referrals, and low-vision rehabilitation.
“Although AMD is a local disease, we believe it is influenced by systemic inflammation,” says Anne Lynch, MD, MSPH, professor and director of the Division of Ophthalmic Epidemiology. “The eye is a sensitive target of that inflammation.”
“The development of an AMD progression risk score that combines established AMD risk factors, significant new systemic inflammatory profiles, imaging, and genetics, will hasten a personalized approach to the management of intermediate-stage AMD.,” Lynch continues.
The longitudinal study using the patient registry is ongoing, with almost 1,700 patients currently enrolled. Researchers are also recruiting AMD patients in the Denver metro area who may receive care elsewhere.
While the study serves as a reminder of the importance of mental health, CU researchers ultimately hope their work will lead to early identification of a high-risk group of individuals for targeted preventive or therapeutic interventions to interrupt the natural progression of AMD.
“People who have vision loss should be screened for depression and anxiety,” Patnaik says. “The sooner these problems are treated, the better their quality of life will be.”
.png)
.png)

.png)
.png)
.png)
