Faculty in the University of Colorado Department of Ophthalmology are working to prevent physician burnout before it even begins through a new resident wellness program.
“More and more studies show that physician burnout rates are much higher than I think most of us expected,” says Cara Capitena Young, MD, assistant professor of ophthalmology at the university and medical director for the Sue Anschutz-Rodgers Eye Center operating rooms. “The best way to create change is to teach them when they're early in their career.”
The resident wellness program is designed to provide an interactive and engaging learning experience that is built into residents’ basic science curriculum. After completing their internship year in the University of Colorado Department of Internal Medicine, residents can begin the two-year program, which features educational experiences from panels and speakers to active occupational wellness sessions that discuss ergonomics, work life balance, contract negotiations and more.
Capitena Young and Mariam Ahmad, MD, also an assistant professor in the department, lead the program and say it comes at a critical time, as more ophthalmologists increasingly report symptoms of burnout.
Prevalence of burnout in ophthalmologists
A 2020 survey, the largest of its kind, conducted by faculty in the CU Department of Ophthalmology, found that more than one in three ophthalmologists feel symptoms of burnout, which is often described as mental, emotional, and even physical exhaustion brought on by repeated or prolonged stress.
“In one survey, ophthalmology was third from the bottom in terms of burnout rate amongst all our colleagues in medicine, but even the specialty with the lowest rates still had a 42% burnout rate,” explains Leonard Seibold, MD, professor of ophthalmology and director of the department’s glaucoma fellowship, who led the survey. “That's a significant amount.”
Factors such as loss of autonomy, increased time spent charting, cramming more patients into tight clinics, doing more with fewer staff, declining reimbursements, and changing regulations and oversight are all reasons why ophthalmologists say they are feeling the effects of physician burnout.
“Because we've gotten so good at restoring vision, especially with cataract surgery, we’re now dealing with even more patients who are achieving 20/20 vision, but may still be unhappy,” Seibold says. “Expectations have sometimes become unreasonable and that's a very difficult thing to deal with.”
The survey of nearly 600 ophthalmologists also found that women are at a higher risk of experiencing burnout, as are physicians who work in a hospital or academic setting, compared to being in a small or large private practice group.
The resident wellness program seeks to reduce those burnout statistics and help prepare future ophthalmologists with the tools to do so.
“Programs have more recently started to realize that burnout and mental health can have an effect on patient outcomes, the structure of the department and general happiness,” Ahmad says. “We’re hoping to improve not only the learning environment for residents, but also for their patients.”
The six dimensions of wellness
The resident wellness program, which officially launched in July 2021, is focused around the six dimensions of wellness — emotional, occupational, physical, social, intellectual, and spiritual — developed by Bill Hettler, co-founder of the National Wellness Institute.
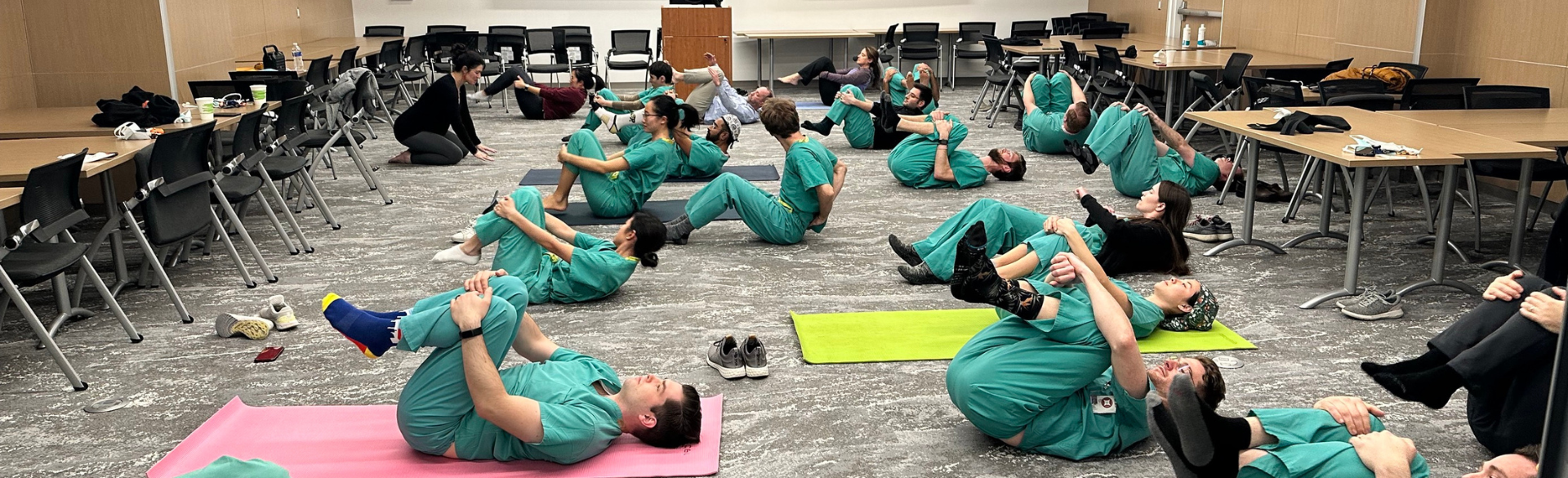
Sometimes the lessons include classic self-care mechanisms such as yoga, but they also focus on issues specifically relevant to ophthalmologists, such as improving ergonomics during surgery.
“More data is coming out about how poor our ergonomics are in ophthalmology, from operating at the microscope to using the slit lamp to doing retinal lasers. Positions we stay in while performing surgery are not good for our necks and upper backs,” Capitena Young says. “The number one cause of disability and early retirement among ophthalmologists is neck and back pain, so it’s important that we’re paying attention to this.”
 Residents in the Department of Ophthalmology get a lesson in ergonomics. |
Other lessons have included panels that focus on other aspects of stress, like managing finances and landing a job. Residents attend a lecture based on one of the six elements for an hour once every few months and then complete assignments, which range from readings and quizzes to activities that boost morale.
Some assignments are voluntary, such as giving compliments to other residents, but intend to boost overall confidence and connection with their peers. The program concludes with a resident retreat that focuses on team building.
|
Residents from the Department of Ophthalmology participate in a field day at the end of the wellness program. |
Ahmad and Capitena Young say they hope the program can be an example for other departments and residency programs.
“While we were putting this program together, we read a lot of the materials for the first time ourselves and learned so much,” Capitena Young says. “I'd love to see this wellness program expand into the department and see more wellness in general across the university through working together with other programs.”






.png)