Researchers in the Department of Ophthalmology at the University of Colorado School of Medicine have received nearly $4 million in R01 grants from the National Institutes of Health (NIH) to move forward in their work at CellSight, the Ocular Stem Cell and Regeneration Research Program based at the Sue Anschutz-Rodgers Eye Center.
The grants, which are supported by the National Eye Institute (NEI), allow researchers continue their mission of one day being able to restore vision to patients experiencing irreversible blindness due to diseases such as age-related macular degeneration (AMD).
Valeria Canto-Soler, PhD, associate professor of ophthalmology and director of CellSight, was awarded $2.1 million over four years to develop solutions to support cell-based transplantation strategies to regenerate photoreceptors and retinal pigment epithelium (RPE) cells, which work together in processes involved in light detection and visual function.
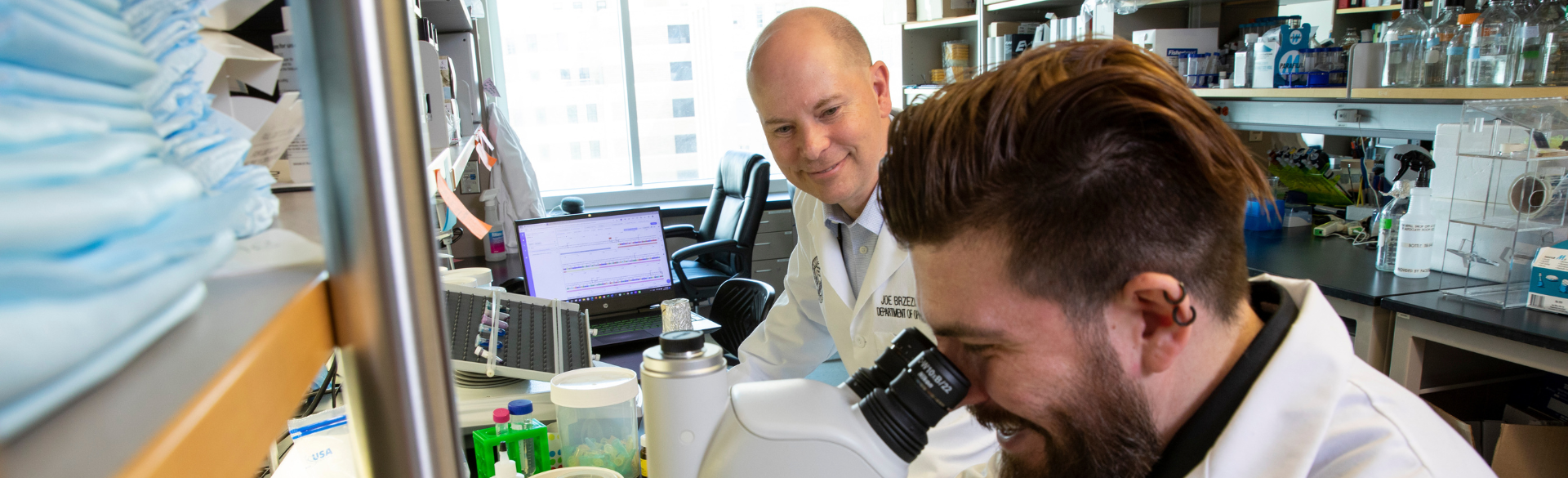
Joseph Brzezinski, PhD, associate professor of ophthalmology and director of CellSight’s laboratory of developmental genetics, received $2 million in an R01 grant renewal that supports his research into understanding how different types of cells in the retina are formed. This work helps build the foundation for designing treatments that may one day help cure AMD-related blindness.
“Restoring vision in AMD patients is a big dream, but we are continuously moving closer to that being a reality,” Canto-Soler says. “These grants along with our passionate CellSight team could help accomplish something truly incredible that we believe could one day make a difference in so many lives.”
Understanding the blueprint for building the retina
The retina needs several types of cells to function properly.
“Everybody has heard of rods and cones, but the retina is made up of several other kinds of cells, too,” Brzezinski says. “Each of these cells are crucial for vision, and our goal is to understand the genetic blueprint responsible for building each of these cell types.”
Gene regulatory networks control how the cells are formed, establishing their types and proportions to enable vision. Through the NIH grant, Brzezinski aims to understand how multipotent progenitor cells choose to become photoreceptors versus other types of neurons. Understanding this key piece of retina functionality could unlock a world of discovery in the future.
“As a basic scientist at heart, I want to know how everything works. How do you put together this giant genetic blueprint that builds a tissue? As we uncover these developmental mechanisms, we can leverage this information to help treat blinding diseases,” Brzezinski says.
A functional foundation for transplantation
There is currently no available treatment that can restore lost vision caused by end-stage dry-AMD, but that may change through Canto-Soler’s work.
“To address this important unmet need, we need to address two critical gaps: devising novel cell-based transplantation strategies to jointly regenerate photoreceptors and RPE cells, and then identifying mechanisms driving structural and functional integration of the transplanted cells,” she explains.
Her project aims to fill those gaps.
In order to restore vision in a patient that has lost the photoreceptors, it’s necessary to replace those non-functioning photoreceptors with healthy photoreceptors. They also need to establish connections with the cells in the retina and transmit the signal all the way back to the brain. AMD patients tend to lose RPE cells first, so the NIH-funded project aims to identify mechanisms that successfully allow the transplantation of stem cell-derived 3D retinal transplants containing photoreceptors and RPE in an animal model with end-stage outer retina degeneration.
Having already developed a transplant using human-induced pluripotent stem cells, the goal is now to find ways to successfully transplant them into the retina to help an AMD patient regain vision.
“By May 2028, when this grant concludes, I hope that we’re able to demonstrate that these cells can become structurally and functionally integrated into a retina,” she says. “This will give us important pre-clinical data that we hope will pave the way to a clinical trial in human patients and, eventually, fulfill our dream of restoring vision in these patients.”



.png)