A newer technique for preparing corneal tissue for transplantation has been shown to be safe and effective, while providing a faster and smoother process than the traditional technique, according to researchers in the Department of Ophthalmology at University of Colorado School of Medicine.
Cornea transplantation has long been an option for patients with vision impairments stemming from cornea problems. In recent years, partial-thickness corneal transplantation, or Descemet’s membrane endothelial keratoplasty (DMEK), has emerged as an effective treatment for patients with Fuchs’ dystrophy, a condition in which endothelial cells – which line the inner layer of the cornea – die off. During DMEK surgery, the surgeon only removes and replaces the damaged inner layer of the cornea, which decreases risks of transplant rejection and offers potential for excellent vision.
“It’s a great procedure because it has wonderful visual outcomes and a much lower risk of transplant problems down the road compared with older transplant techniques,” says Karen Christopher, MD, assistant professor of ophthalmology in the CU School of Medicine and lead author for the study recently published in the journal Cornea. “It can really restore vision-related quality of life for patients who suffer from symptoms of Fuchs' dystrophy, and our research shows we can do this more successfully now than ever before.”
 A donor cornea is pictured at the Rocky Mountain Lions Eye Bank.
A donor cornea is pictured at the Rocky Mountain Lions Eye Bank.
Christopher notes that it can be a challenge to prepare and transport the corneal transplant tissue, which is as thin as a sheet of plastic wrap, and endothelial cells may die in the process. The procedure has been refined since its advent in 2006, with new tools developed specifically for tissue removal and transport.
Christopher led the CU research team comparing different approaches to preparing cornea tissue for DMEK transplantation – one using a relatively new tool called the DMEK EndoGlide and one using a tool called a Jones tube, modified from a glass tube that had been used in tear drainage surgery. The research was conducted at the Rocky Mountain Lions Eye Bank, which partners with about 120 hospitals in Colorado and Wyoming to recover donated eye tissue for use in transplants, research, and training. The eye bank prepared and then gathered data for 30 DMEK grafts used in the study.
“Most people don't realize that besides facilitating ocular donation for research and transplant, the eye bank also prepares the grafts for specific transplant procedures, such as DMEK, for the surgeons prior to surgery,” says John Lohmeier, executive director of the eye bank. “The study results confirm that our preparation practices are cutting edge and effective.”
The EndoGlide technique preserves the tissue in a tiny capsule and forceps are later used to pull the tissue into the eye during surgery; it performed comparably to the modified Jones tube technique, which has been used for DMEK surgery for many years.
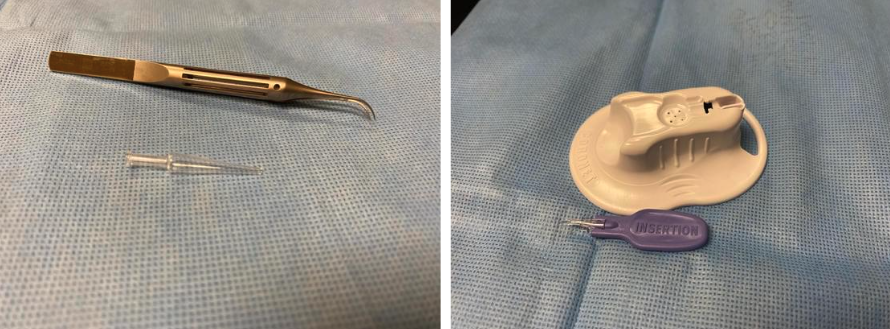 Cornea tissue for DMEK has long been prepared using a "modified Jones tube" (left) until the EndoGlide (right) was developed specifically for the procedure. CU researchers compared both techniques in a recent study.
Cornea tissue for DMEK has long been prepared using a "modified Jones tube" (left) until the EndoGlide (right) was developed specifically for the procedure. CU researchers compared both techniques in a recent study.
Christopher says this is the first direct comparison of Jones tube with the EndoGlide technique, which she says provides more control for the surgeon during the transplantation, leading to faster and more regulated tissue implantation – and likely better long-term outcomes.
She credits the team at Rocky Mountain Lions Eye Bank, located at the Sue Anschutz-Rodgers Eye Center, for its role in the research.
“We have a great partnership with the Rocky Mountain Lions Eye Bank,” Christopher says. “Not only do they provide us with excellent quality cornea tissue and meticulously prepare it for DMEK transplantation, they also are on the forefront of developing new techniques such as this one. Without them our surgical successes would not be possible!”
In 2021, the eye bank facilitated the donation of tissue from 2,450 donors, from which 316 corneas were used in DMEK procedures. In its 40-plus year history, this nonprofit organization has facilitated the recovery of more than 58,000 eye tissues for transplant and 15,000 eye tissues for research, training, and education.

.png)


.png)