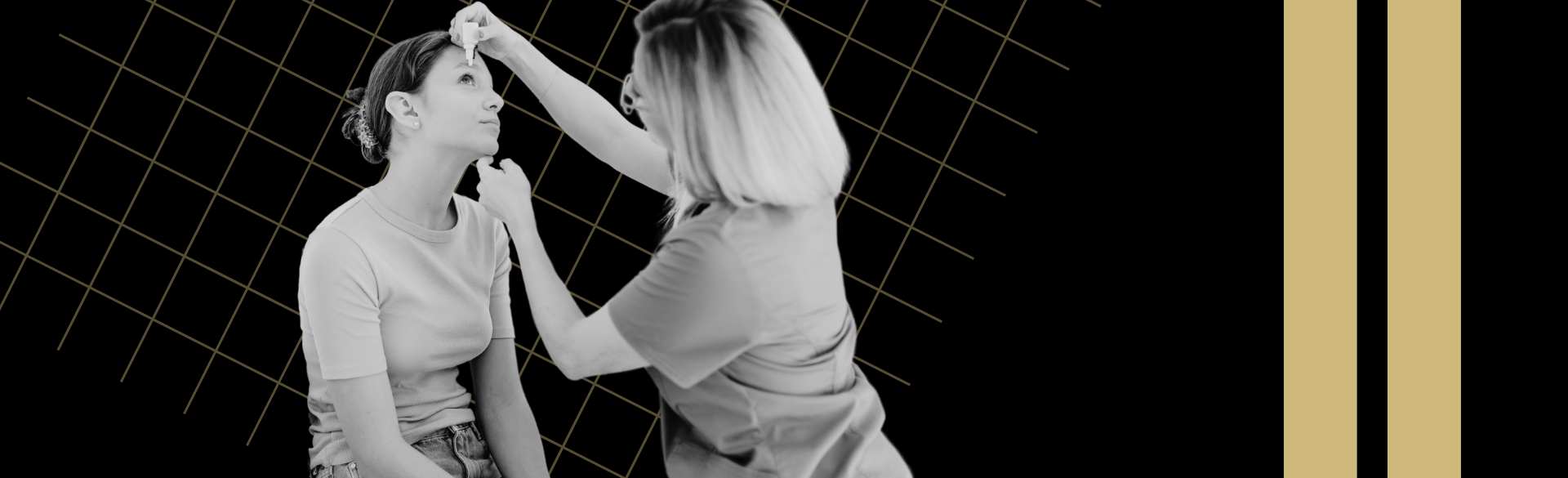
While eye drops are often a helpful treatment mechanism that deliver necessary medications to the ocular surface, they can also present challenges for some patients.
Ophthalmologists and eye specialists at the Sue Anschutz-Rodgers Eye Center count irritation, physical limitations, and compliance among the most common obstacles they say patients encounter. In older patients with glaucoma, squeezing a small eye drop bottle may be difficult, and having many different drops to manage an ocular condition can make it challenging to stay on top of a regimen.
Some patients with glaucoma also face more noticeable side effects, including increased dry eye, when they begin eye drop medications.
“It’s not uncommon to have difficulties with eye drops,” says Monica Ertel, MD, PhD, assistant professor of ophthalmology at the University of Colorado School of Medicine, who often helps her patients find solutions to obstacles associated with eye drops.
Ertel encourages patients facing challenges with eye drops to talk to their ophthalmologist. There may be an aid or device that may make delivering the medications a bit easier and more manageable.
Finding the right aid
Earlier this year, Ertel took to the web to find as many eye drop aids as she could that patients could potentially purchase online. They ranged from silicone guides that help an unsteady hand place the drop in the correct spot to plastic devices that act like bulky tweezers that help the patient squeeze the eye drop bottle.
“We have a small fraction of patients who struggle with drop administration,” Ertel says. “As you can imagine, these little drop bottles are tough plastic, and sometimes the preservative-free drops are in little individually wrapped vials that require micro-manipulation to pull the top off and squeeze the bottle to administer.”
 A selection of eye drop aids Monica Ertel, MD, PhD, has found online. Neither Ertel nor the department have financial interest in these products.
A selection of eye drop aids Monica Ertel, MD, PhD, has found online. Neither Ertel nor the department have financial interest in these products.
In glaucoma patients, medicated eye drops help slow down progression of the disease by lowering intraocular pressure (IOP) and sometimes require multiple doses throughout the day. Keeping up with drops is crucial, but trouble administering them can mean a patient puts them off or takes them less often, which could lead to disease progression and the need for more invasive treatments.
In searching for aids online, Ertel says she was surprised at how many are available and the range of challenges they target. Among her most interesting finds is a flat piece of plastic outfitted with several holes. The patient is to tilt their head back, lay the plastic above their eye, and place the bottle in one of the holes to administer the drop.
“These devices might not work for everybody, but they are be a helpful option for a patient who needs a good guide to help them get the eye drop into their eye,” she says.
Other devices can help reduce the size of the drop, which can be helpful when a patient has a medication that is costly and needs to make the most of each drop. The device screws onto the cap of the bottle and limits how much medication is released. Ertel says most drops are significantly bigger than the eye can hold, so it doesn’t prevent patients from getting the amount they need.
Beyond physical challenges
Aids make drops more physically accessible, but compliance can remain an issue for some patients.
“Some of the biggest obstacles to the proper use of prescribed topical therapeutics are generally related to human factors that are almost impossible to overcome,” says Malik Y. Kahook, MD, professor of ophthalmology and the Slater Family Endowed Chair in Ophthalmology.
Forgetfulness and motivation can play a big role in adherence — even with alarms, digital reminders, and tips for motivation. This is driving the need for more creative solutions so that patients have a better chance of managing their ocular condition and preserving their vision.
READ MORE: How eye drops are used to treat ocular health conditions
Developing new delivery tools
The bevy of obstacles that patients face with drops has prompted faculty members across the CU Department of Ophthalmology to start thinking about drop delivery differently and what can better serve patients. That might be an aid to help deliver the drops, or it might not be a drop at all.
“I believe that we need a new paradigm for the use of medications for treating eye diseases such as glaucoma. We need therapies that are physician guided and patient independent, thus guaranteeing 100% adherence,” Kahook says.
Toward that goal, Kahook developed SpyGlass, a novel drug delivery platform that’s showing promising results in its first human study. The device, which can deliver IOP-lowering medication for up to three years, is injected into the eye’s capsular bag at the time of cataract surgery, making it more convenient for patients.
In the future, the device could be a gateway to treating other ocular conditions that require drops, too.
“I believe the future of medical therapy for glaucoma isn’t reliant upon patients alone,” Kahook says. “I also believe this will be the case for several other eye related diseases, such as allergies and dry eye, that we treat every day in our clinics.”