Already regarded as one of the country’s leaders in CAR T-cell therapy, University of Colorado Cancer Center member M. Eric Kohler, MD, PhD, has received a $150,000 Scholar Award from the American Society of Hematology (ASH) to investigate a method to make CAR T cells function even better.
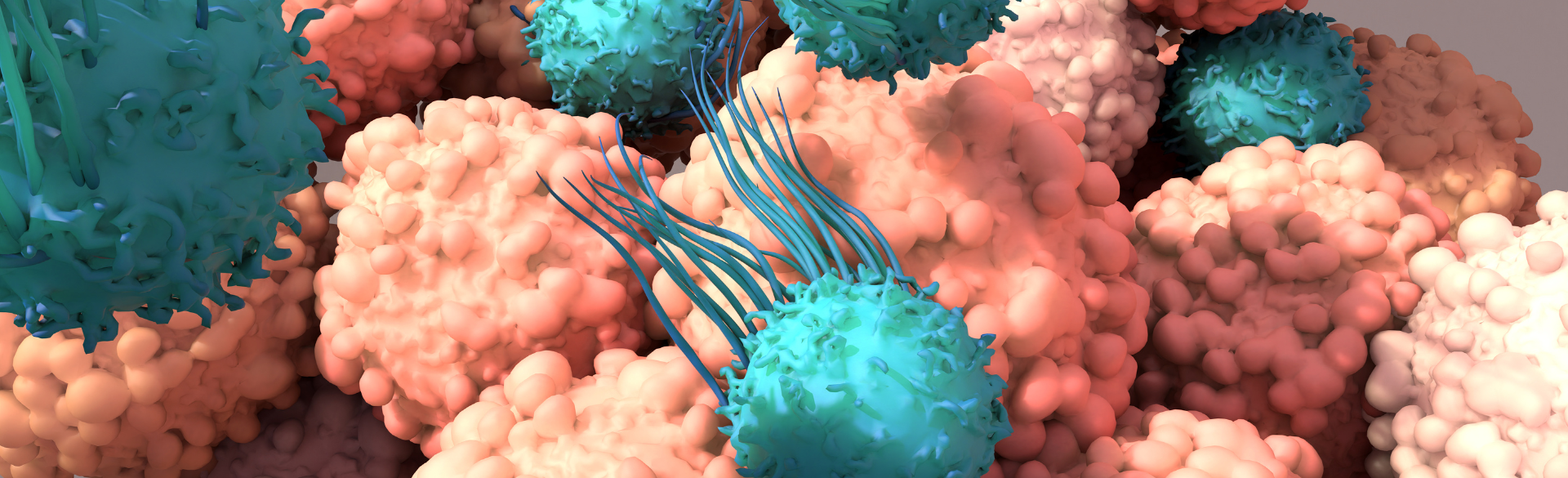
CAR T-cell therapy works by removing immune cells known as T cells from a patient’s body through a blood draw and engineering them in a laboratory to target specific molecules on cancer cells before returning them to the patient’s bloodstream. One problem that arises with CAR T therapy, Kohler explains, is that the engineered immune cells often aren’t able to target tumor cells with low levels of the target molecule.
His research into the issue resulted in the creation of a new type of CAR cell that is able to more effectively go after tumor cells with lowered levels of the target protein.
“What we’ve done is to develop a completely new design for the CAR molecule. This design came from studying why the original would fail,” says Kohler, provider at Children’s Hospital Colorado. “We identify a molecule called LAT as a choke point in the activation signal from the CAR molecule. To overcome this choke point, we built a CAR that specifically signals through the LAT molecule and amplifies the signal in the CAR T cell. When we did that, we were able to target tumor cells that have really low levels of the target molecule on their surface.”
Investigating toxicity, longevity
In the two-year study funded by the ASH Scholar Award, Kohler plans to look at whether the new therapy — dubbed ALA-CART (adjunctive LAT-activating CAR T cell) — lasts longer in the body. The study will also examine if the new design increases the potency of the CAR T cells without increasing the toxicity of the treatment.
Since tumor cells can decrease the amount of their targeted proteins to evade CAR T cells, the ability of CARs to target low levels of the molecule is a problem that needs to be solved to make the therapy more effective and long-lasting.
“Current CAR therapies rely on the LAT that naturally exists in the T cells before they are turned into CAR T cells,” Kohler explains. “But there is nothing in the design of standard CARs to cause these two molecules to interact. Nature didn’t design LAT to find our CAR molecules, and CAR molecules weren’t designed to bind LAT. In our ALA-CART format, we actually put more LAT into the T cell, and we force the interaction of the CAR and the LAT so we can restore that signal that's been missing.”
New hope for treatment of blood cancers
Targeted at patients with blood cancers such as leukemia, the ALA-CART therapy may eventually help patients in whom previous CAR T therapies have failed. In the case of leukemia, the CAR is specifically targeted at a protein known as CD22.
“When patients get CAR T cells targeting CD22, they often respond really well initially,” Kohler says. “Unfortunately, many relapse shortly after, because the leukemia reduces the amount of CD22 on the surface of the cell to a low level that the CAR can’t target. Those patients usually have very few treatment options left. If our new ALA-CART works the way we think it will, we’re hoping it will be an effective long-term therapy for patients.
Valuable support
Based on his preliminary data, Kohler says, the ALA-CART format is likely to work better against all target proteins, not just CD22, and the boosted immune cells will stay in the body for a longer period of time, making the patients much less likely to relapse. He is grateful to ASH for giving him the means to further explore the new treatment.
“It’s huge to have this kind of support and receive funding for this project,” Kohler says. “We are going to keep building and keep pushing toward a clinical trial. It’s a very competitive award, so it’s a really nice nod to get it. It’s going to help move this project forward over the next couple of years, which I hope will ultimately improve patient outcomes.”