The good news for people with multiple myeloma is that treatments exist that almost always put the cancer into deep remission soon after it’s diagnosed. The bad news for people with the blood cancer, though, is that even though that remission can last several years, almost all patients eventually relapse — and the disease that returns becomes increasingly difficult to treat.
“We have a lot of different drugs that work well, but none of them cure the disease,” says University of Colorado Cancer Center member Dan Sherbenou, MD, PhD. “When patients relapse, they have progressively shorter lengths of time in remission, and they never get to the same depth of response they got from their first line of therapy. Eventually they develop a relapsed and refractory disease that is resistant to all the best drugs we have, and that’s usually when a patient suffers mortality from their disease.”
Funds for investigation
Sherbenou recently received a Research Scholar Grant from the American Cancer Society to investigate the causes of drug resistance in multiple myeloma, with an eye toward developing clinical trials of various methods to overcome the resistance.
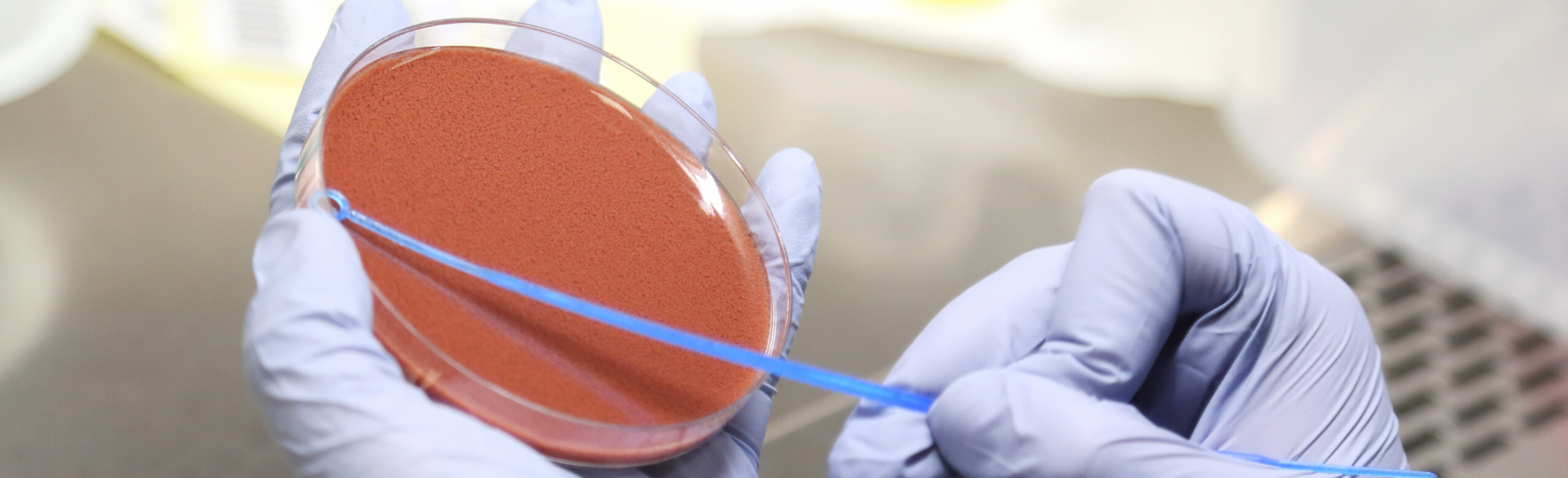
Using patient samples and a novel ex vivo detection tool called Myeloma-Drug Sensitivity Testing, or My-DST, Sherbenou and his research team plan to look at resistance to three important types of treatment for multiple myeloma: immunomodulatory drugs, proteasome inhibitors, and chimeric antigen receptor T cells (CAR T cells). In addition to profiling the patient samples’ resistance to current drugs, researchers also will test their sensitivity to new drugs that could be used to treat relapses when they happen.
“Tumors are heterogeneous, multiple myeloma included,” says Sherbenou, associate professor of hematology in the CU School of Medicine. “We want to see if resistance to these drug classes is detectable at an early stage of development, when it’s at a subpopulation level. We will simultaneously look at gene expression and profile protein drug targets on the surface and inside of individual myeloma cells, to distinguish resistance pathways that might not yet be detectable at the level of the bulk tumor.”
Re-targeting resistance
In each type of resistance, Sherbenou says, he plans to look for new targets that can yield new sensitivities in the resistant myeloma cells. In the case of immunomodulatory drugs, for instance, he hypothesizes that the oncogene known as MYC helps the cancer cells avoid the effects of the treatment, while on the other hand tumors that grow to be resistant to proteasome inhibitors have high levels of the protein CD138.
“Right now we don’t have an immunotherapy that targets CD138, but that would be something that would be relatively easy to do if CD138 is present at high levels on resistant cells,” he says.
For patients who develop resistance to the relatively new CAR T cell treatment, Sherbenou will look for low expression of a protein called B cell maturation agent (BCMA), the primary target of CAR T cells in multiple myeloma, as well as high expression of CD38, a protein targeted by monoclonal antibody drugs. Many patients start CAR T after monoclonal antibodies targeting CD38 are no longer effective, but Sherbenou’s group has found that in those patients, the resistance to CD38-targeting drugs eventually fades.
““We’re hypothesizing that CD38 is a target that increases in expression after CAR T,” he says. “But we don’t think going after it again with a monoclonal antibody is going to be the right approach. Instead we'll use a T cell-engaging antibody to exploit the target and avoid cross resistance.”
Developing trials
Once all the testing is complete, Sherbenou plans to develop clinical trials of each of the new drugs his team finds to be successful in overcoming resistance. It’s an important next step in a cancer that is growing in prevalence.
“Around 2% of all cancer patients have multiple myeloma,” he says. “The incidence has aggressively increased over the last several years. And because we’re keeping people alive longer, the prevalence of the disease is growing rapidly as well. We have an aging population worldwide, which means people are living longer and at risk of developing cancers in general. Since multiple myeloma is a cancer of primarily older people, it’s becoming a huge health problem.”
Sherbenou is grateful for the ACS grant that recognizes the importance of his work and gives him the funding to conduct this vital research.
“It’s a big step for my lab, and hopefully we will contribute to better understanding of drug resistance and better understanding of other treatments that will be effective in that relapsed and drug refractory patient,” he says. “We ultimately still need to figure out a way to cure this disease, but now that I’ve got this ACS support, it will allow me to continue my mission of developing model systems where we can better characterize residual disease.”