What is the problem you were looking to address with this research?
One of the biggest challenges with T cell-based immunotherapy is that it relies on the ability of the cancer cell to display foreign antigens on its surface. A protein is made inside the cancer cell, then it's broken up into small pieces, and those small pieces are detected on the surface. Now, it's up to the immune system to determine whether those new peptides are foreign or not. That’s how the immune system determines whether it's an intruder or not an intruder. About 40% of melanoma patients don't respond to these types of immunotherapies, and then you have some who are not long-term responders. The idea is that in these cancers that don’t respond to immunotherapy, can we make them more visible to the immune system?
What have you learned about why some of those patients fail to respond to immunotherapy?
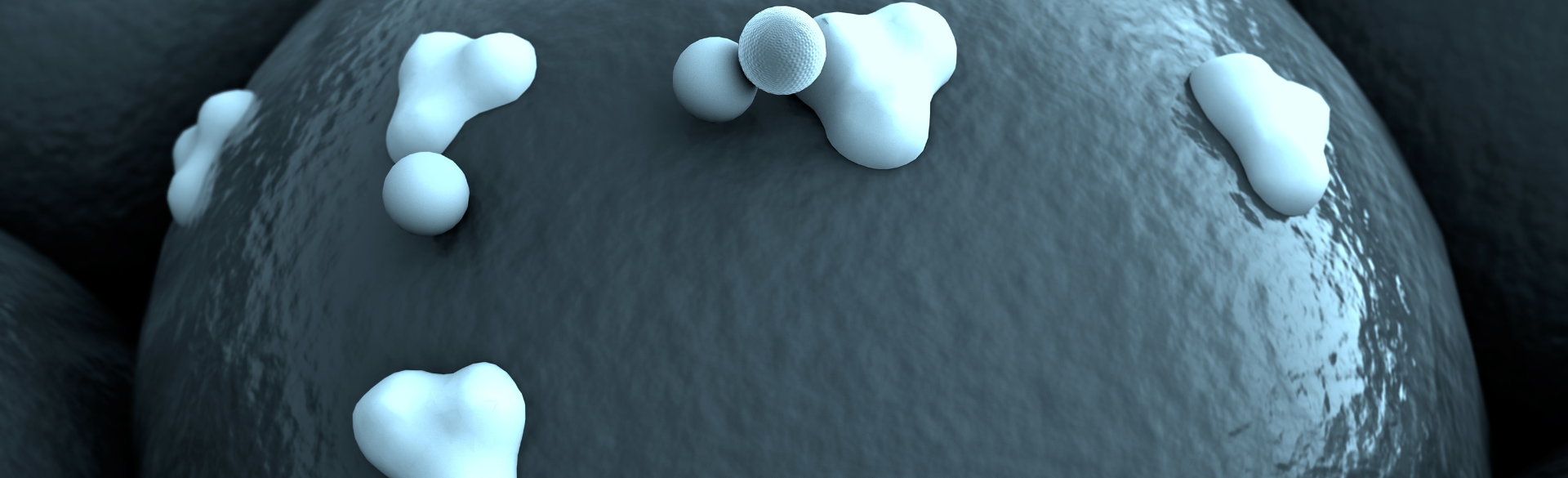
Cancer cells have a lot of mutations, and if those mutations translate into a change in the amino acid of a protein that is properly presented on the surface of the cell, then the immune system has the potential to be activated against that. Those proteins are called neoantigens, because they're new antigens. One of the reasons a lot of T cell-based immunotherapies fail is that the cancer cells either don't express a lot of these mutations as a protein, or the cancer cell has found a way to reduce the display of these antigens on the surface.
Is there a way to make those proteins more visible to the immune system?
One of two things could help in that scenario: Either you coerce the cancer cell to express more of these proteins on the surface, or you transcriptionally regulate the expression of new genes in a cancer cell. A cancer cell might only express 10 neoantigens on the surface, but if you can somehow find a way to coerce it to express 10 times more than that, in theory, you should have a stronger immune response or at least give the immune response a bigger chance at detecting that cancer.
Several years ago, we screened about 3,000 different drugs for the ability to modulate the expression of a protein called MHC-1, which presents proteins to a T cell. From a screen of about 3,000 different drugs, we found five drugs that did what we wanted them to do, which is increase MHC-1 and reduce the expression of other proteins. This R01 is based on the novel idea that we have discovered a new signaling pathway that coerces cancer cells to expose more antigens and express more MHC-1 proteins. These cells found a way to escape detection by the immune system, but we found a drug and a mechanism that shifts their abilities. We found that we're able to increase not only the levels of neoantigens that are presented, but also a much broader spectrum of neoantigens.
Was this drug originally designed to make cancer patients more vulnerable to immunotherapy?
No, not at all. We attempted to find another use for drugs that are approved for completely different things. We just asked the question, “Can any of these 3,000 drugs do something different?” It was a shotgun approach, just to see if something cool might happen. We were lucky that a few of the drugs did what we wanted them to do.
What will the funding from the R01 grant allow you to do?
To receive the grant, we had to convince the reviewers that our theory was sound. Now we can start actually performing the experiments. We've generated animal models to test this drug and look at T cell responses, antitumor activity, and tumor growth. We're also looking at whether we can develop prognostic markers or even diagnostic markers for tumor cells that aren’t likely to respond to immunotherapy. Does the expression level of this MHC-1 help predict which patients are going to respond?
So far, are you finding that the new drug helps?
Yes. Our drug combination — the new drug plus the immunotherapy — works great. We're able to restore the activity of the immune system now. A lot of the tumor samples that we work with are basically incurable — we get no response in animal models, and humans don't respond well to the immunotherapy alone. But once we start using the combination therapy, you can see the tumors just melting away.