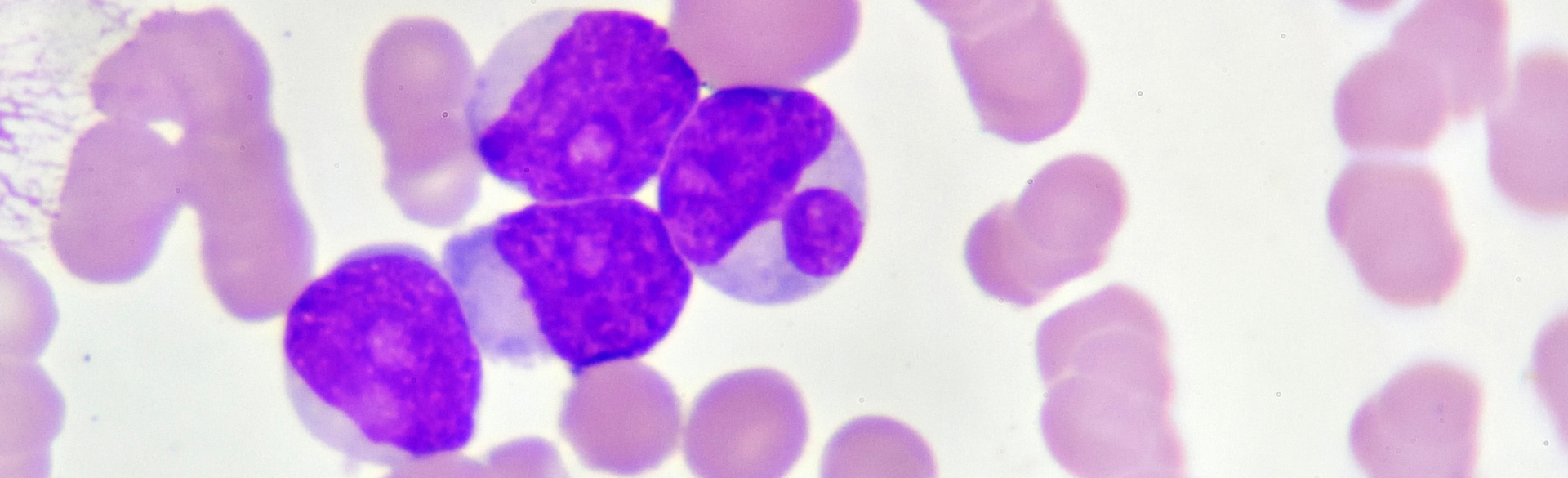
New research conducted in the lab of University of Colorado Cancer Center co-deputy director James DeGregori, PhD, may explain why acute myeloid leukemia (AML) cells that reside in the bone marrow are more resistant to medication than AML cells found in the blood and elsewhere in the body.
“The bone marrow is the home of the leukemia,” says DeGregori, professor of biochemistry and molecular genetics in the CU School of Medicine. “If you don't get rid of the cells in the bone marrow, you're not getting rid of leukemia. There are drugs that achieve effective responses in the periphery, but they are not effective in the bone marrow itself.”
Discovering a new pathway
Analyzing data in DeGregori’s lab for his thesis research, now third-year medical student Hae “Harry” Park, PhD, discovered why that resistance happens. His research showed that supportive cells within the bone marrow called stromal cells are activating a signaling pathway known as mammalian target of rapamycin (mTOR) in the AML cells, making them resistant to a standard AML therapy known as a FLT3 inhibitor. Mutation of the FLT3 gene is common in AML, and this mutation encourages the growth of too many abnormal white blood cells; a FLT3 inhibitor targets the mutation to stop the abnormal growth.
“Other research has shown that if you take stromal cells from the bone marrow, they can provide protection from not just FLT3 inhibitors, but almost any drug you can think of,” DeGregori says. “Bone marrow is known to be protective against drug insults. Harry has figured out a whole pathway as to why that is.”
In a paper published October 19 in the journal eLife, Park, DeGregori, and the rest of the research team showed that an mTOR inhibitor and a FLT3 inhibitor, when taken together, had a profound effect on AML cells in animal models.
“Our group was pleasantly surprised to discover that the addition of an mTOR inhibitor to a FLT3 inhibitor not only significantly reduces the leukemic burden in the bone marrow, but also prevents the relapse that usually occurs with FLT3 inhibitor monotherapy,” Park says.
Further testing showed that the leukemia cells within the bone marrow only need the support of the stromal cells when they are “under attack” from the FLT3 inhibitor and need the mTOR pathway activated.
“All of the signaling is happening in the AML cell, so in the lab we can even just take the media that the stromal cells make, add it to the AML cells with the FLT3 inhibitor, and see the pathway get activated,” DeGregori says. “The role of stromal cells is to make something that that is protecting the AML cells.”
Next stop, humans
For the next step in their research, DeGregori and Park hope to begin a clinical trial of the drug combination in humans, using FDA-approved FLT3 and mTOR inhibitors to stop the spread of AML in the bone marrow. It could be a huge step forward in treatment for AML, a blood cancer that starts in the bone marrow and can spread to other parts of the body including the liver, lymph nodes, spleen, and central nervous system. AML occurs most often in adults, and according to the American Cancer Society, in 2022 there will be about 20,050 new cases of AML and about 11,540 deaths from AML in the United States.
“We believe our research provides a strong rationale for moving forward to clinical trial,” Park says. “Given that mTOR inhibitors are generally well-tolerated, we believe that mTOR inhibitor in combination with FLT3 inhibitor would benefit patient outcome by effectively reducing the leukemic burden in the bone marrow and thus prevent relapse.”