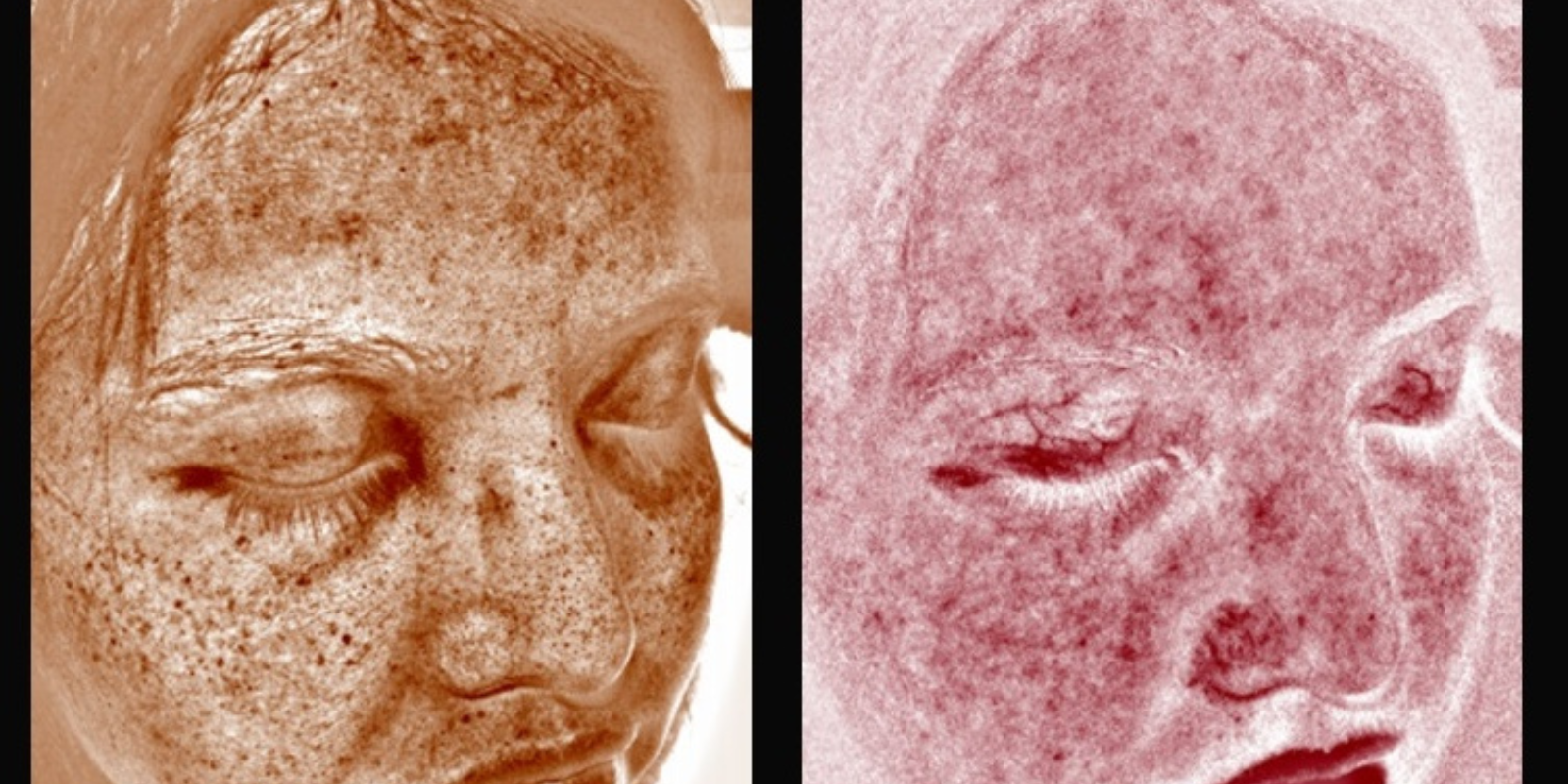
In melanoma, myeloid-derived suppressor cells (MDSCs) are bad – the more MDSCs, the poorer a patient’s prognosis. That’s because when these MDSCs expand to accumulate near melanoma tissue and in blood circulation, they suppress the immune system so that it doesn’t attack the cancer. But how do MDSCs expand and how do they accumulate near melanoma tissue?
A University of Colorado Cancer Center study published in the journal Frontiers in Oncology hints at an answer. Chemicals in the body called interleukins regulate the immune system, in large part deciding concentrations and locations for the various types of immune cells. The current study shows that the interleukin called IL-6 may help to grow MDSCs, while another called IL-8 may recruit MDSCs toward tumor tissue. Of course, melanoma makes both IL-6 and IL-8. But drugs already exist to block the action of IL-6 (developed primarily in the context of rheumatoid arthritis), and drugs are in development to block IL-8, speeding the possibility of new therapeutic options against melanoma, should ongoing work support the current results.
“This is building on some work we had done showing that melanoma patients with higher MDSC concentrations had poorer outcomes. But we didn’t know if it was chicken or egg – were MDSCs driving melanoma or was the melanoma inducing more MDSCs? This takes it to the next level, showing a functional role for IL-6 and IL-8 in driving melanoma outcomes,” says Martin McCarter, MD, CU Cancer Center investigator and surgical oncologist at the UCHealth University of Colorado Hospital.
The study compared factors in the blood of 55 stage IV melanoma patients with 22 healthy controls. Importantly, the study followed up with these patients 5-7 years after treatment, allowing the researchers to correlate blood factors with survival. Basically, this design allowed the researchers to ask two questions: What is different between the blood systems of people with melanoma and those without, and which of these differences seem important to a patient’s survival?
“If you only look at the short term picture, you only get one side of things, namely what’s different in the blood of melanoma patients. With long-term follow up, we can show which factors actually mean something to long term survival,” McCarter says. “What we found is that if IL-6 stays low and MDSCs stay low, no matter how you do it or what treatments you use, these low levels correlate with better survival.”
McCarter points out that the study even outlasted some of its original researchers, including Kimberley Jordan, PhD, who started the project and is now assistant director of the Human Immunology and Immunotherapy Initiative at the CU School of Medicine, and postdoctoral fellow Richard Tobin, PhD, who saw the project to completion.
“This paper establishes that melanoma can make IL-6 and IL-8 and that levels of these interleukins correlate with concentrations of MDSCs in the tumor and the circulation. IL-6 can stimulate the growth of MDSCs and IL-8 can attract MDSCs to tumor tissue. We hadn’t been able to put that story together before. This puts a direct link from these interleukins through MDSCs to outcomes,” McCarter says.
The work supports the rationale of ongoing investigator initiated clinical trials offered at CU Cancer Center using all-trans retinoic acid (ATRA) to reduce MDSCs, as a promising treatment for stage IV melanoma.