Newly published research by Eduardo Davila, PhD, associate director of cancer research training and education coordination (CRTEC) at the University of Colorado Cancer Center, identifies a new method for helping a patient’s immune system successfully attack cancer cells.
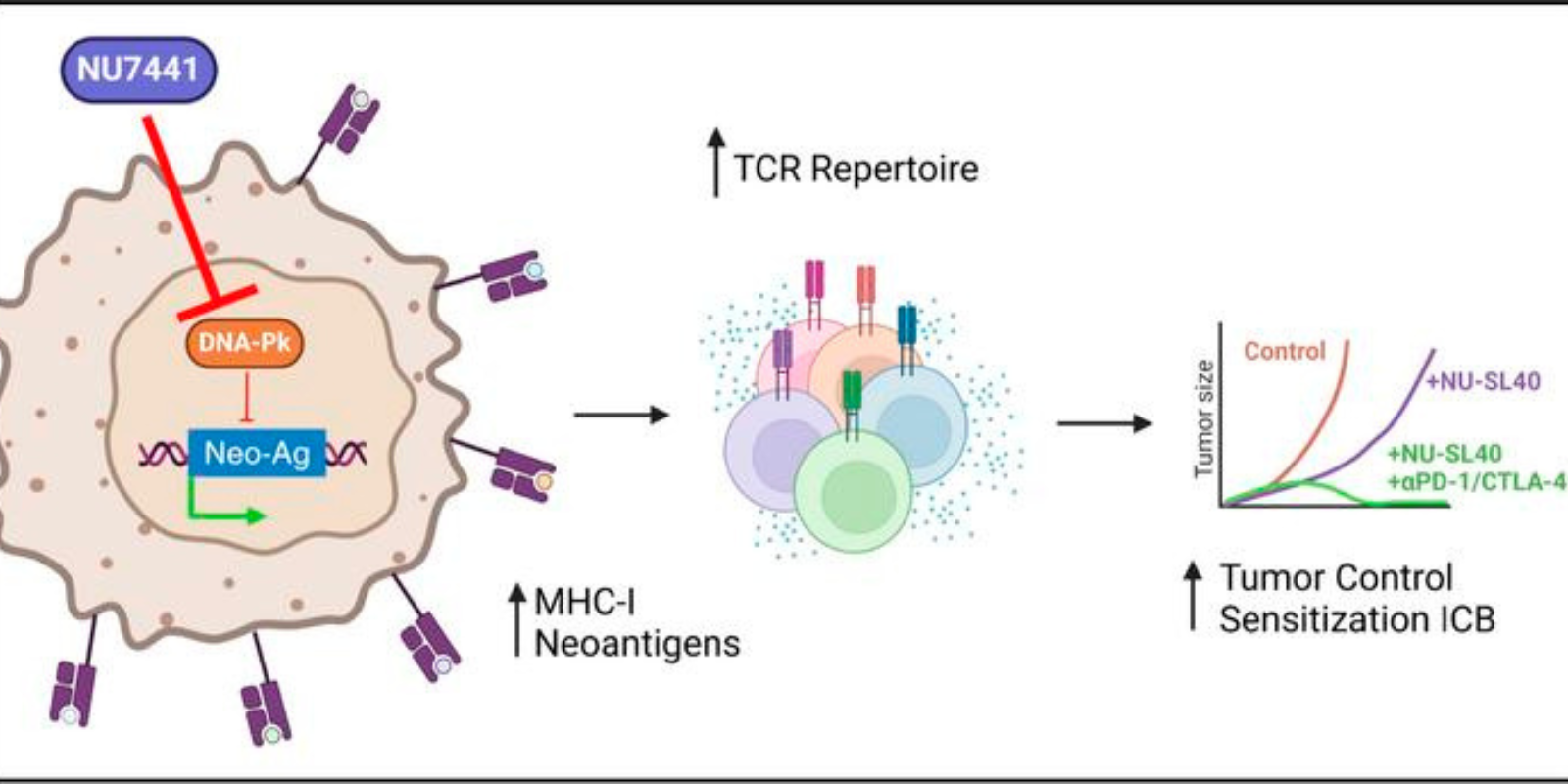
Published in this fall in the Journal of Clinical Investigation, the research specifically finds that a type of drug known as a DNA-PK inhibitor can inhibit a tumor cell’s ability to evade T cell detection by preventing targetable molecules from appearing on the surface of a cancer cell.
“We conducted a drug screen of about 3,500 different FDA-approved drugs to see if any of them could make the cancer cell a better target for cytotoxic T cells,” Davila says. “What we found is that when we administered the DNA-PK inhibitor, the T cells were able to destroy a tumor that normally isn't destroyed because it's resistant.”
Inhibiting inhibition
Subsequent research by Davila and his team found that the DNA-PK inhibitor is so effective because it blocks the activity of the DNA-PK protein, which normally causes a tumor cell to stop producing the MHC molecules as well as inhibit the expression of tumor targets known as neoantigens that cause it to be detected and attacked by T cells.
“We found that DNA-PK serves as a stop signal, so it stops the production of these MHC molecules, and it stops the production of neoantigens that are usually presented as a way for the immune cell to recognize the cancer,” Davila says. “That was completely unheard of until we made this observation. What we found is that we can restore the enhanced anti-tumor activity of these immune cells through a mechanism that wasn't discovered before. Not only does it restore the expression of the MHC molecules, but it increases the expression levels of these molecules, making the tumor cell more visible to the immune system.”
Enabling immunotherapy
That increased visibility, Davila says, not only boosts the ability of the immune system to fight cancer cells, but it also enhances the efficacy of multiple forms of immunotherapy, including checkpoint inhibitors, tumor-infiltrating lymphocyte (TIL) therapy, and T cell receptor engineered therapy. Davila’s research focused specifically on melanoma cells, but he thinks the findings may be applicable to other types of cancer as well.
“We discovered a drug, we discovered a new mechanism, and we discovered a way to enhance the activity of several types of immunotherapies,” he says. “That sets the foundation for moving this into clinical testing for patients who are not responding to immunotherapies. The question is, can we pretreat or combine treatment for these patients with a DNA-PK inhibitor, plus any of these checkpoint or T-cell therapies to restore their activity by making the cancer cell more visible and making these T cell responses more robust?”
Future testing
Davila has already met with melanoma specialist and CU Cancer Center member Sapna Patel, MD, to talk about using the DNA-PK inhibitor with patients; he also is talking with the pharmaceutical company that manufactures the drug about moving forward with clinical trials.
“Melanoma is one of the prevalent cancers in Colorado, due to our increased sun exposure, so this addresses one of our cancer center’s unmet needs in melanoma,” he says. “But others in the medical oncology field here — the doctors on my floor who treat different types of cancers such as GI cancers, pancreatic cancer, and breast cancer — are also interested to see whether this drug combination can benefit their patients.”
Predictive science
Davila’s research additionally found that DNA-PK can be used as a biomarker to determine if patients are likely to respond to the combination of the inhibitor drug and immunotherapy. If a blood test detects the presence of DNA-PK in its activated — or phosphorylated — state, a provider will be able to predict a patient’s response to the treatment.
“Depending on what other protein it interacts with, I can tell whether it's going to block or promote the expression of the neo-antigens,” Davila says. “We might be able to use that as a predictive mechanism to determine whether they're even going to respond to immunotherapies at all.”