For years, David Albers, PhD, associate professor of biomedical informatics at University of Colorado School of Medicine, has been haunted by a friend’s death. It was long before Albers contemplated a career in health care, when he was an undergrad studying physics and taking music lessons in his spare time from accomplished jazz musician Tony Williams.
When his musical mentor died of a heart attack in 1997 at age 51 – as an inpatient following routine surgery – Albers was shocked. He came to believe that Williams, a Black man, didn’t receive medical intervention in a timely manner despite alerting care staff that something didn’t feel right, a sentiment frequently voiced by patients across the health care system.
“He went in for gallbladder surgery, and he left in a body bag,” Albers recalls. “It probably wasn’t malicious bias, but hospital staff just didn’t listen.”
.png?width=283&height=377&name=Tony%20Williams%20(450%20%C3%97%20600%20px).png)
Tony Williams, 1945-1997.
Data mining the electronic health record
Albers, now a biomedical informaticist who builds computational models, believes an AI-powered predictive tool he helped build would have made a difference in Williams’ care and that of countless other patients. He believes it would address institutional hierarchies built on a culture of unquestioning trust in doctors, as well as unintended bias in patient care.
The Communicating Narrative Concerns Entered by RNs (CONCERN) Clinical Decision Support (CDS) system is integrated into the electronic health record (EHR) and assigns a numerical score that is input into a user interface and associated with green, yellow, or red status indicating not at risk of deteriorating, at risk of deteriorating, or already deteriorating, respectively. During shift changes, the scores help the care team flag patients who might be at risk of declining. Additionally, CONCERN surfaces nursing expertise to the rest of the interdisciplinary care team.
That tool was implemented at four hospitals affiliated with two health systems – Partners Healthcare System in Boston and New York Presbyterian Health System in New York – in 2019 and a three-year study of the program was launched. Albers and the other authors of the study noted that the tool would address the systematic problem in hospitals of “non-optimal communication between nurses and doctors leading to delays in care for patients at risk.” They focused on mortality attributed to cardiac arrest and sepsis and hypothesized that many of the deaths are preventable if at-risk patients are detected earlier.
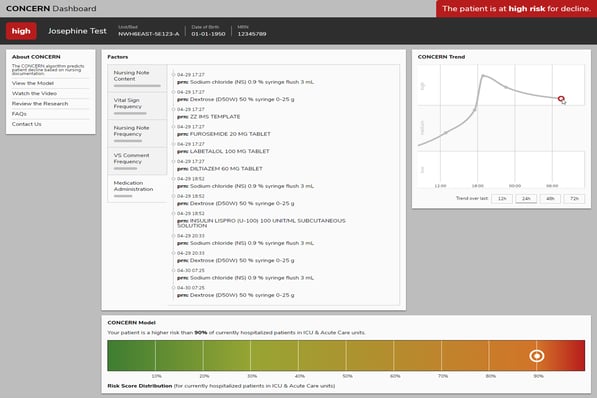 The dashboard from the CONCERN clinical decision support tool indicating a hypothetical patient is at high risk of deteriorating. The project received grant funding from the National Institute of Nursing Research and American Nurses Foundation.
The dashboard from the CONCERN clinical decision support tool indicating a hypothetical patient is at high risk of deteriorating. The project received grant funding from the National Institute of Nursing Research and American Nurses Foundation.
A complete analysis of the results from the study that concluded in November 2022 are pending, but results from the trial indicate a significant reduction in mortality. Discussions are ongoing to bring the CDS tool to UCHealth University of Colorado Hospital.
‘Nurses love it’
The work on CONCERN began over a decade ago, when Albers was on the faculty at Columbia University and initiated discussions about health care processes with two nurses trained in informatics – Kenrick Cato, RN, PhD, and Sarah Collins Rossetti, RN, PhD. Albers spoke to them about Williams’ case, which led to discussions about similar cases.
“Out of that came the discussion that nurses probably notice things before it shows up in the data,” Albers says, surmising that nurses often observe subtle changes in patient behavior or appearance that doctors may not notice. When nurses’ concerns are raised, they will take vital signs and perform other tests with increased frequency. These observations are recorded in patients’ EHRs and are represented by the health care process, but such information is often overlooked because of fragmented information displays, “note bloat,” and information overload.
“It’s the documentation patterns that matter much more than what’s being documented,” Albers says. “For instance, if the nurses are not worried about you, they’re not going to wake you up at 2 a.m. to take your blood pressure.”
Although Albers envisioned the computational machinery in the CDS, he credits Cato and Rossetti, who served as principal investigators on the CONCERN study, for spearheading the initiative and for their deep collaboration with the methods development. Additionally, Christopher Knapland, a data scientist, contributed substantially to the model development.
“It took a carefully integrated and highly interdisciplinary team to develop methods and teamwork frameworks for incorporating clinical expertise with the data science pipeline such that an impactful CDS tool could be created,” Albers says.
“When we were implementing CONCERN, the idea was that it would help nurses push on the hierarchy by giving them a tool that rank orders patients empirically,” he adds. “The nurses love it because it’s saving lives.”



.png)
