What is your background with robotic surgery?
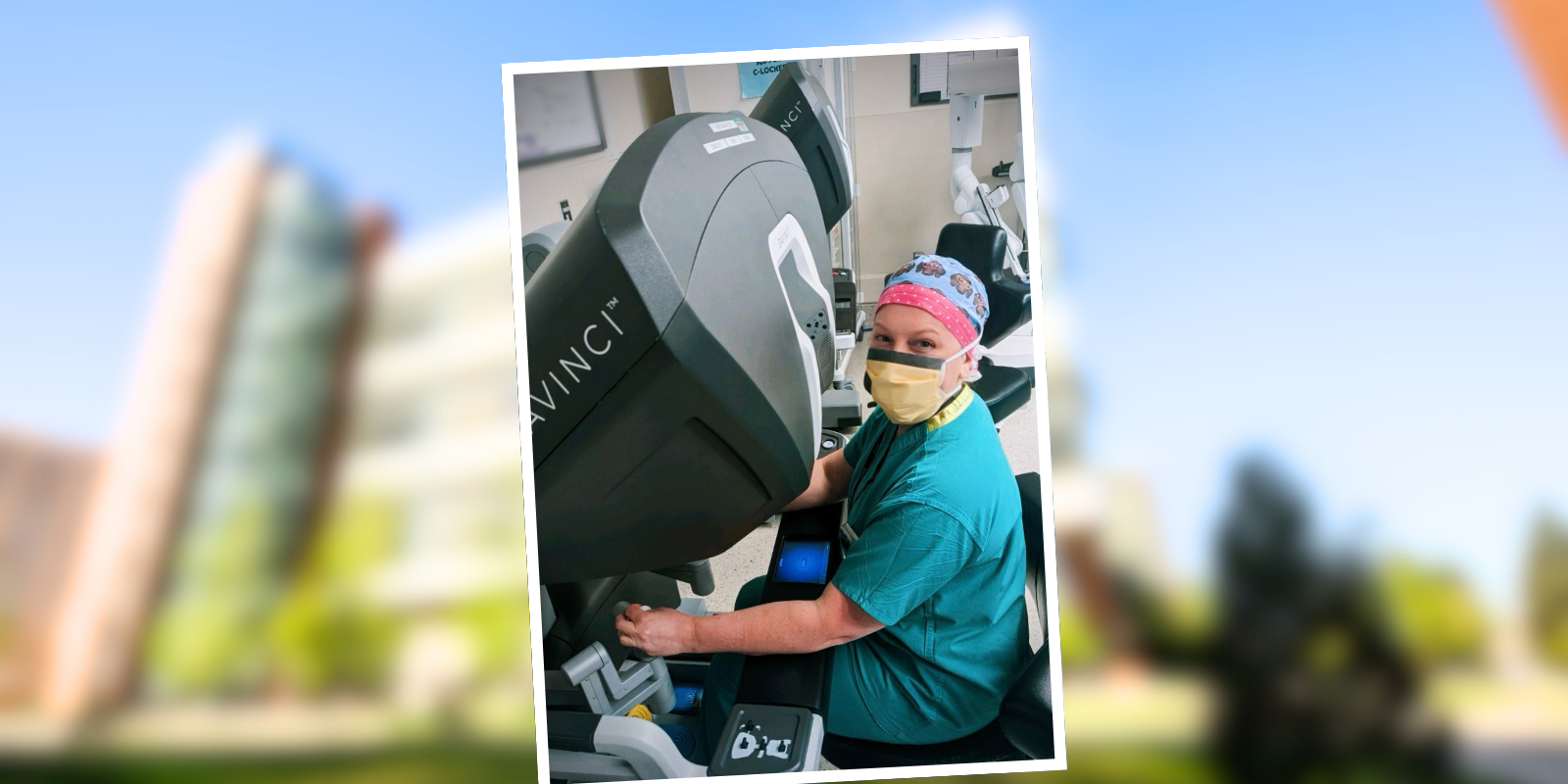
My training was mostly in robotics, and I had 24/7 access to a robot during my residency. Then I did a trauma fellowship, which was mostly focused on open trauma cases. I've been an employee at the University of Colorado for just over a year, and I am the director of robotic surgery education for the general surgery residency program.
What is your role with robotic surgery within TACS?
I am the only surgeon in the TACS department who is currently credentialed to perform robotic surgeries. Other trauma surgeons are interested in completing the requirements and offering this surgical option for ideal candidates. We’re making a case to the administrators that we want to offer the same standard of care independent of the time of day. It shouldn't matter if it's an emergency case or if it's in the middle of the night — if the surgeon feels that the procedure should be robotically performed or that the patient would benefit from it, we are lobbying for that access. The progress we have made to date has been possible due to the support of the hospital administrators and OR staff.
What was the specific situation with the patient who had the robotic emergency cholecystectomy?
The patient had acute chronic cholecystitis, meaning they had had this pain for a long time. I suspect that because of their high weight, and because the condition wasn't emergent at that time, the patient was not offered surgery in the community. When they came into our ED, I heard about the patient’s situation, and I thought, ‘That's going to be really challenging to do laparoscopically; let's see if we can do it robotically.’ I had submitted all my paperwork, so all I needed to do was to find a proctor — the hospital requires that another surgeon who's actively doing robotic surgery at the University watch our first three cases. I had to arrange a time when the robot was open and the proctor was available. All the stars aligned, which allowed me to perform the first TACS robotic case.
What makes it easier to do that surgery robotically on someone with a high BMI?
People hold their weight differently. Patients can have intra-abdominal fat or a thick abdominal wall, or both. And when a patient has a very thick abdominal wall, if you're operating laparoscopically with straight instruments, you're pushing down or lifting up on this very heavy abdominal wall. It's physically challenging to operate on patients with high BMI. With the robot, the surgeon is not physically applying the torque on the abdominal wall, and the instruments have fully wristed articulation. Now I'm sitting comfortably at a console, at my perfect ergonomic level, and I'm just using my hands to work the controls. There's not an assistant who is retracting and physically exerting pressure on the heavy abdominal wall.
Beyond the actual physics of it, you get a much crisper, better view with the 3-D camera that’s attached to the robot. The camera doesn't fog up, like our laparoscopic ones, and you're able to have better visualization in contaminated or inflamed surgical fields. With the super high-definition camera – it’s just hard to compare with traditional laparoscopic surgery.
How did the emergency cholecystectomy surgery go?
It went well. We were able to schedule the robot in less than a day, the surgery took 73 minutes to perform, and the patient was discharged within 24 hours. While the use of robotic technology in emergency general surgery is becoming more prevalent nationally, early studies have demonstrated it may be associated with better patient outcomes as measured by reduced conversion to open surgery and decreased hospital length of stay.
How are emergency robotic surgeries scheduled?
The current process is if there’s a patient that I feel would benefit from robotic surgery, I work with the OR managers to see when a robot will be available. Sometimes, there are cancelations for the elective robotic surgeries — maybe a surgical oncologist wants to do a case robotically, and they go in, and there's metastatic disease, so they decide not to do the surgery at that point. Or maybe the patient cancels last minute. They try to work us in when there's availability. I did my first robotic evening case at 8 p.m. the other night because the OR could accommodate me that evening for a patient who was seen by our service at 5 p.m. in the emergency department.
What needs to happen to make emergency robotic surgeries more common?
It's not as simple as, ‘Kristy Hawley wants to do this.’ The robot has to be available. Anesthesia has to be available. Most importantly, the OR staff must be available to make it happen. We need somebody to exchange the robotic instruments. We need somebody who feels comfortable bringing the robot in when we're scrubbed to dock the robot. We are working to make sure that all the staff are robotically trained and prepared to perform robotic surgeries at all hours of the day. We're not quite there yet, but that's the goal. As we continue to see growth in the use of robotics in all surgical specialties, including mine, we will continue advocating for robotic access for emergency surgery for our patients.