2023 was an exciting year at the University of Colorado, resulting in 85 blogs covering the research, education, and provider care that has been performed over the past months. Our stories this year featured faculty, researchers, and patients as they exemplified the incredible work being accomplished by the Department of Surgery, including a revolutionary transplant surgery and new departmental leadership.
Here are the top stories of 2023 for the Department of Surgery.

The Bachelor in Paradise 'Poo Baby,' Explained
It was one of the most dramatic moments in “Bachelor” franchise history. And it wasn’t about a love triangle or an early departure or who would get a rose — it was about whether contestant Sam Jeffries could go to the bathroom.
Last week’s episode of “Bachelor in Paradise” ended on a cliffhanger as Jeffries — who hadn’t had a bowel movement in nine days — was told by on-set medics that if her situation didn’t improve, she would have to go to an operating room for a procedure to “deliver” her “poo baby.”

What Breast Cancer Patients Can Learn From Suzanne Somers’s 23-Year Battle
Actress Suzanne Somers, best known for her iconic role as Chrissy Snow on the 1970s and ’80s sitcom “Three’s Company,” died October 15 after a 23-year struggle with breast cancer. Somers was 76.
In June 2023, Somers revealed in an Instagram post that her breast cancer had returned, writing that “I had breast cancer two decades ago, and every now and then it pops up again, and I continue to bat it down. I have used the best alternative and conventional treatments to combat it. … This is not new territory for me. I know how to put on my battle gear, and I’m a fighter.”
We talked with Gretchen Ahrendt, MD, professor of surgical oncology, about what a 23-year battle with breast cancer looks like and what other people with the disease can learn from Somers’s experience.

CU Surgeons Set Records for Transplants in 2022
2022 was a record-breaking year for the number of transplants performed by the organ transplant team at the University of Colorado Department of Surgery, with more than 300 kidney transplants, more than 130 liver transplants, more than 60 heart transplants, and 40 lung transplants performed over the past 12 months.
“We’re one of the largest transplant programs in the U.S. — and certainly the largest in this region,” says Elizabeth Pomfret, MD, PhD, chief of the Division of Transplant Surgery and the Igal Kam, MD, Endowed Chair of Transplant Surgery. “It’s been a big ask from the OR, because the vast majority of organs that we transplant are from deceased donors, so we need to have the operating rooms immediately available when we get the organs. It’s really an institutional effort, because we end up bumping a lot of other cases for the transplants. Unfortunately, every organ has a finite amount of time that it can be outside of the body before irreversible damage occurs, resulting in an organ that does not function.”

Smoking and Surgery: Why the Two Don’t Mix
Doctors are always trying to convince their patients to stop smoking, but it’s a concern that’s especially vital prior to surgery, due to the effects smoking has on the body.
“Patients who smoke are at a higher risk of a heart attack during or just after surgery, because smoking causes constriction of the blood vessels,” says Simran Randhawa, MBBS, assistant professor of cardiothoracic surgery in the University of Colorado Department of Surgery. “Smoking also is known to inhibit wound healing and cause problems with general anesthesia, and it can contribute to postoperative complications such as pneumonia and lung infections.”
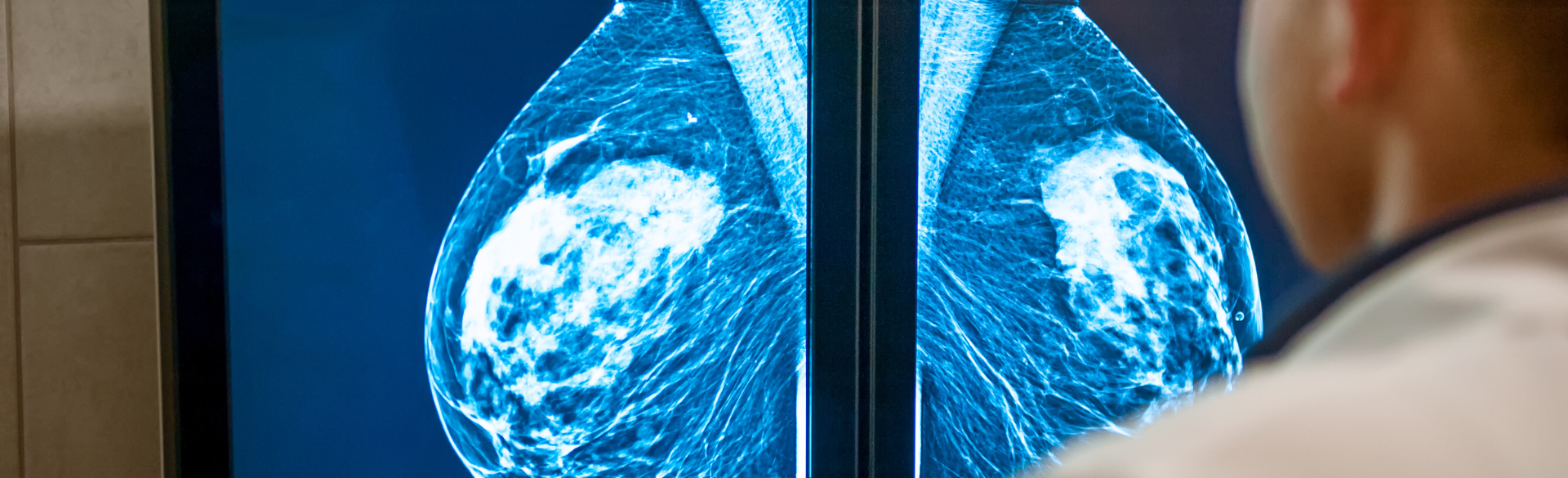
FDA Issues New Mammography Guidelines for Women With Dense Breasts
For women with dense breasts, getting a mammogram to screen for breast cancer can be something of a double whammy. Not only is cancer more difficult to detect in dense breasts, but dense breasts also are a risk factor for developing breast cancer in the first place.
“A lot of women think that if their mammogram is negative, they don’t have cancer,” says Gretchen Ahrendt, MD. “But the test is only as good as your breast density. The higher your breast density, the harder it is to find a cancer.”
In an effort to help more women with dense breasts understand their screening options, the Food and Drug Administration (FDA) on March 9 updated its mammography guidelines to require mammography facilities to notify patients about the density of their breasts. The new rule amends regulations issued under the Mammography Quality Standards Act of 1992, a law passed to ensure quality mammography. The amendments are required to be implemented within 18 months.

Division of Pediatric Surgery Welcomes New Chief
Today, the Division of Pediatric Surgery in the University of Colorado Department of Surgery welcomes a new chief, one who brings a strong commitment to growing diversity and equity in pediatric surgery and supporting surgeons as research scientists.
Ankush Gosain, MD, PhD, joins the division from the University of Tennessee Health Science Center, where he served as vice-chair for academic affairs, senior surgical advisor for quality and safety, and director of surgical research.
Gosain made the decision to come to Colorado because “it’s a really exciting opportunity,” he says. “Children’s Hospital Colorado is a top five children’s hospital widely recognized for clinical excellence, and the Division of Pediatric Surgery is the same. When I look at the people in the division – faculty, advanced practice providers, and staff – there’s so much talent and so much potential there."

CU Surgeons Perform Department’s First Robotic Living Liver Donation
Aiming to increase the number of living liver donors by making liver donation surgery easier and quicker to recover from, the University of Colorado Department of Surgery recently performed its first robotic hepatectomy (surgery to remove a portion of the liver) from a living donor. Using a surgical robot to perform the procedure results in a smaller incision, less scarring, less pain, and a faster recovery for the donor.
“There are a lot of advantages to using the robot for this operation,” says Trevor Nydam, MD, associate professor of transplant surgery, who led the team that performed the first robotic surgery at CU. “Once you get through the learning curve and you're able to fully use the robot, the visualization is excellent. The technique allows us to be gentle with the tissue. Our hope is that it helps to remove some of the disincentive to donation, getting people back to work sooner. They don't have to take as much time away from their normal daily life to recover from this.”

Nanoknife Procedure Preserved Prostate Cancer Patient’s Quality of Life
James Bird gets emotional talking about it. How he qualified for a clinical trial that, in his view, preserved his manhood after he was diagnosed with prostate cancer in late 2022.
“The day I went in to see if I qualified, there were 10 other guys out there in the lobby who didn’t get into the trial,” he says. “I felt so sorry for them. One of the technicians who was involved with the trial told me he was getting calls from all over, from guys begging to get in. That’s how important this is.”
The trial, run by Al Barqawi, MD, was for a new procedure for treating prostate cancer. An alternative to the standard-of-care surgery that removes the prostate altogether, the minimally invasive procedure — known as irreversible electroporation (IRE), or Nanoknife, destroys cancer cells within the prostate by running an electric current through the prostate cells and tissue.

New Chief of Cardiothoracic Surgery Brings Commitment to Diversity and Innovation
The Division of Cardiothoracic Surgery in the University of Colorado Department of Surgery has named Joseph Cleveland Jr., MD, as the new division chief.
In his new role, Cleveland brings a commitment to growing diversity, equity, and inclusion in cardiothoracic surgery, supporting surgical research, and increasing the division’s profile locally, regionally, nationally, and internationally.
“We have a high-performing, robust set of programs, everything from end-stage heart failure to structural heart disease, arrhythmia surgery, as well as robust lung cancer and esophageal cancer surgical programs,” Cleveland says. “All of these things are in place, so one of my goals is to take something that is a superb program and work with the incredible talent we have on our faculty to increase our footprint in the Denver metro area and increase what we’re known for as a strong regional program into one of the marquee programs nationally and internationally.”

Enjoying the Gift of Time After a Pancreatic Cancer Diagnosis
Before receiving a pancreatic cancer diagnosis eight years ago – a diagnosis that resulted from persistent self-advocacy – Carolyn Degrafinried spent one awful weekend wondering if she was losing her mind.
Deep down she knew she wasn't, but for a moment it did feel that way – one of cancer’s occasional and cruel side effects. Through that terrible weekend, she had back and stomach pain so severe that she could barely move. By Monday, though, the pain was gone and never returned.
Still, she knew she hadn’t imagined that pain, and she knew something was wrong. So, she asked her primary care provider for whatever tests could help explain what was going on, and an ultrasound showed a mass on her pancreas. The initial diagnosis was that it didn’t look like cancer.
However, for several weeks after she couldn’t ignore her lingering feeling that something was off and requested more testing. This time, in April 2015, an endoscopy showed that not only was the mass on her pancreas a tumor, but it was cancerous.




