What is peptic ulcer disease?
Essentially, an ulcer is a disruption or defect in the mucosa, which is the top layer of tissue in the digestive tract. Peptic refers to the ulcer being related to acid.
And there are two main types of PUD, correct?
Yes. We have gastric, which are stomach ulcers, and duodenal, which are small intestine ulcers.
What are its symptoms?
Classically symptoms are abdominal pain, often upper-abdominal pain, or pain that gets better or worse with food. But it's important to note some people will be asymptomatic or have atypical symptoms, like feeling full quickly, bloating, nausea, or have symptoms of the complications of PUD like vomiting or even bleeding from the GI tract.
Are there any other early warning signs that someone might be able to pick up on that, if caught early, would help lessen severity? When should someone call their primary care doctor about an ulcer?
There aren't any specific early warning signs, but of course patients should pay attention to any new, different, or worsening symptoms that they're having and see their provider early on in that course of their symptoms. We always tell patients: You know your body best.
Essentially, you want to diagnose and treat PUD before you develop any complications, which could be GI bleeding, perforation or even obstructive symptoms from inflammation or scarring from the ulcer.
You can also be proactive. If you are someone who needs high-dose non-steroidal anti-inflammatory medications (NSAIDs) for pain control, talk to your doctor about how you could prevent ulcers, maybe by taking a proton-pump inhibitor (PPI) along with the NSAID, lowering the NSAID dose, or potentially using Tylenol, which is not an NSAID, to help control pain.
What specifically causes peptic ulcer disease?
There are two common causes of PUD. The first is a bacterial infection called Helicobacter pylori (H. pylori). The second is NSAIDs. Those are ibuprofen, Motrin, Naproxen, aspirin-type medications. There are other medications that have been associated with PUD, like steroids or potassium chloride pills, or sometimes it can be associated with diseases that cause high acid secretion, like Zollinger-Ellison syndrome.
Are there any specific risk factors for PUD?
There are a few:
-
Overuse or high dosages of NSAIDs. Sometimes people are on two NSAIDS, like ibuprofen for pain control and a baby aspirin for heart health, which can increase your risk of PUD.
-
Having a personal history of ulcer disease or even a family history of peptic ulcer disease can increase your risk.
-
Cigarette smoking, alcohol exposure, or living in areas that have a high prevalence and transmission of H. pylori.
-
Older age, having liver disease, lung disease, or kidney disease.
Are there any myths related to PUD?
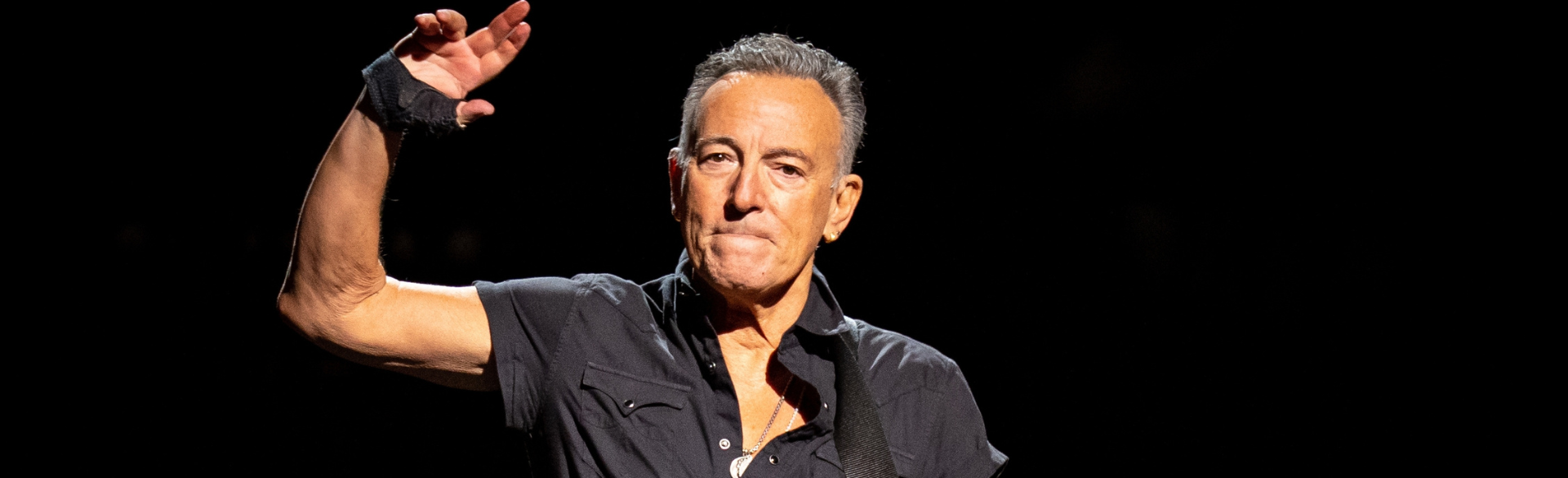
The most common myths are around stress and diet. Ulcers are not caused by emotional stress or by worrying. They're not caused by a poor diet – that you might have when you're on the road as a traveling performer.There are certain foods that can exacerbate the symptoms of an ulcer but don't necessarily cause the ulcer..
Of course, in a very stereotypical way, if a rock star like Springsteen has increased exposure to heavy alcohol or cigarette smoking, that will increase the risk.
How is PUD diagnosed? How do we treat it after a diagnosis?
The most sensitive and specific way of diagnosing peptic ulcer disease is through endoscopic evaluation where you visualize the tissue in the stomach and the small intestine. PUD can also be diagnosed with a barium X-ray that evaluates the mucosa for an ulcer defect. Sometimes patients present with abdominal pain and end up getting a CT scan that shows there may be an ulcer in the stomach or small intestine, seeing inflammatory changes in the area.
Based on those suspicions, we'll move forward to an endoscopy to evaluate for an ulcer. We’ll take stomach biopsies to see if there is an H. pylori infection and get a detailed medical history to see if the patient is on NSAIDs. We try to eliminate those risk factors and treat the underlying cause, treating them with antibiotics to get rid of the infection or decreasing or stopping NSAIDs.
The most common medication that we use to heal these ulcers are proton-pump inhibitors, which are acid-blocker medications, and we generally put patients on a high PPI dose of 40 mg twice daily. Patients will be on high dose PPI for usually six to eight weeks.
If we can't identify a reason for what caused the ulcer, for example if there wasn’t NSAID or tobacco exposure, or if H. pylori biopsies were negative, then we'll generally keep patients on at least a daily dose of PPI indefinitely. If a patient had a gastric ulcer, we repeat the upper endoscopy 6-8 weeks after the diagnosis of PUD to make sure the ulcer is healed. We don’t repeat an upper endoscopy for duodenal ulcers.