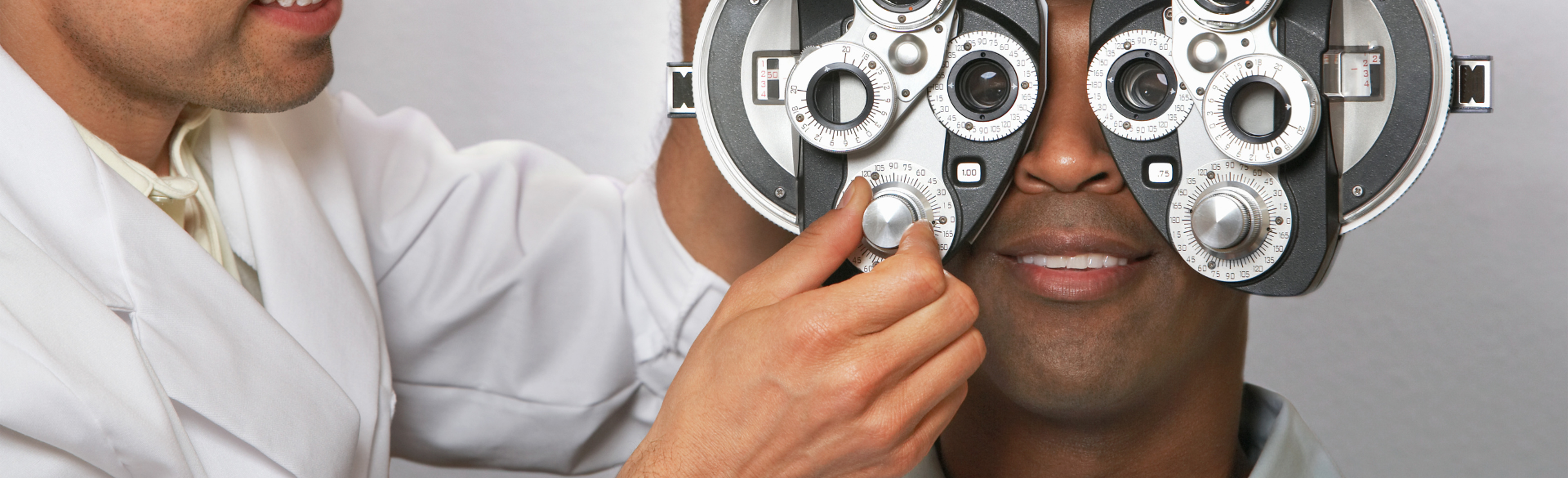
Although Black Americans are the second-largest minority population in the United States, they remain underrepresented in vision health research. They also carry the highest burden of eye disease ranging from general visual impairment to glaucoma, diabetic retinopathy, and blindness.
In 2012, for example, over half a million Black Americans were diagnosed with open-angle glaucoma, and when adjusting for age, were three to four times more likely to have a diagnosis of glaucoma compared to white Americans and two times more than Hispanic people in the United States. Black Americans also have a higher risk of visual loss from diabetic retinopathy compared to non-Hispanic white Americans.
“The cause of this increased incidence in glaucoma and diabetic retinopathy among Black Americans remains unclear,” says Niranjan Manoharan, MD, assistant professor of ophthalmology at the University of Colorado School of Medicine. “It’s clear though that organizations like ours need to encourage and implement improved methods for prevention and screening with underserved populations who are especially affected by these diseases across the nation.”
Access to equal and earlier treatment
Patients with open-angle glaucoma – the most common form of the disease – require escalating levels of treatment, starting with eye drops, lasers, and then surgery. When it comes to conditions like diabetic retinopathy, there is a similar need for progressive treatment. Patients typically start with preventative actions against systemic diabetes, and if they worsen, will need intravitreal injections, retina lasers, and surgery.
“It’s well established that underserved populations, including Black Americans compared to white and Hispanic Americans, have far lower rates of diabetic retinopathy screening,” Manoharan explains. “This leads to more advanced diabetic retinopathy at time of presentation to an eye doctor.”
“We did a study, which was recently submitted for publication, which shows that minority groups and lower socioeconomic groups present with more advanced diabetic retinopathy leading to worse final visual outcomes,” Manoharan continues. “This is why earlier screening is imperative.”
While earlier screening is the best line of preventative defense, numerous barriers still exist – particularly among Black Americans – including socioeconomic disparities, lack of access to quality health insurance, access to proper care, time, and transportation. Systemic factors also pose obstacles, often including prolonged waiting times for appointments, and general difficulties scheduling appointments.
Eliminating barriers and increasing inclusion
Centers for Medicare & Medicaid Services (CMS) can impose financial penalties to health care providers and health systems for scoring poorly on health screening metrics that include diabetic retinopathy screening, but Manoharan believes we should go further.
“Primary care physicians, health care systems, and government policies are working to improve prevention and screening, but we aren’t really targeting our minority and underserved populations who have the lowest rates of screening and preventative care,” he says. “Tele-retinal screening, especially in the form of artificial intelligence-based screening could be the future. AI-based screening Eyenuk was approved by FDA for diabetic retinopathy screening and is likely to be approved for open-angle glaucoma. We could use these to target these populations who have difficulty accessing care.”
Naresh Mandava, MD, professor of ophthalmology and chair of the Sue Anschutz-Rodgers Eye Center, serves on the board of the Association of University Professors (AUPO) and emphasizes the organization’s mission on diversity, equity, and inclusion, and the responsibility that leaders in the field of ophthalmology have to addressing and implementing solutions that create real change.
“We must continually ensure and increase access to equal quality of care regardless of what a person’s background is,” Mandava says. “It is up to us to set a positive example for the Rocky Mountain region and beyond.”
.png)



