For the millions of Americans who have cloudy and blurry vision due to cataracts — a common condition where the lens of the eye becomes cloudy — they may debate whether to get cataract surgery. However, a cataracts diagnosis does not necessarily mean surgery is required, explains ophthalmologist Michael Wildes, MD.
Wildes is the clinical director at the Sue Anschutz-Rodgers Eye Center and an assistant professor of ophthalmology at the University of Colorado Anschutz School of Medicine. A cataract surgeon and cornea specialist, he completed his residency and fellowship training at CU Anschutz and has extensive expertise in caring for patients with vision loss. Before his patients decide whether they want to proceed with cataract surgery, he makes sure they consider several factors.
“Just because you have cataracts doesn’t mean you need to have cataract surgery immediately,” Wildes says. “While symptoms for cataracts will get worse over time, I always tell patients that we can start the process for surgery if they are bothered by their symptoms — but I don’t want patients to jump into a surgery because they feel like they have to.”
Three things to consider
Cataracts can occur at any age, but the condition is commonly associated with older adults. According to the Centers for Disease Control and Prevention, an estimated 20.5 million Americans aged 40 and older have cataract in one or both eyes — a major issue considering it is the leading cause of vision loss in the nation, with the most severe cases causing blindness if left untreated.
Some people compare having cataracts to looking through a dirty windshield. This blurry and clouded vision can especially impact a person’s vision at night, leading to glare issues.
However, cataracts can vary in severity and do not affect everyone in the same way, which is why Wildes encourages his patients to consider three things before opting for surgery. The first is determining whether a cataract is present and is significant enough to cause vision impairment.
The second is assessing how much the procedure may improve their vision. This is important because there are many other reasons a patient may be experiencing vision loss.
“Usually, when people have 20/20 vision, unless they have a major issue with glare and cannot drive, I often advise that they wait for surgery since we won’t be improving their overall vision much,” Wildes says. “Every person has different needs for their vision. Some can be very bothered by minor cataracts, while others can function very well with more advanced cataracts. While cataract surgery is very safe, there is some risk involved. Therefore, when to do surgery is a decision that varies from person to person.”
The third — and most important — factor a person should consider is how much cataracts are affecting their life, he explains.
“If it is just a minor annoyance but you can still do all the things you need to do, it’s fine to wait,” he says. “Most people get surgery when it reaches the point where it’s starting to impair their ability to do things like driving, especially at night.”
The surgical process
Cataract surgery involves making a small incision through the front of the eye, removing the natural lens that has clouded over time, and replacing it with an artificial lens to restore a person’s vision.
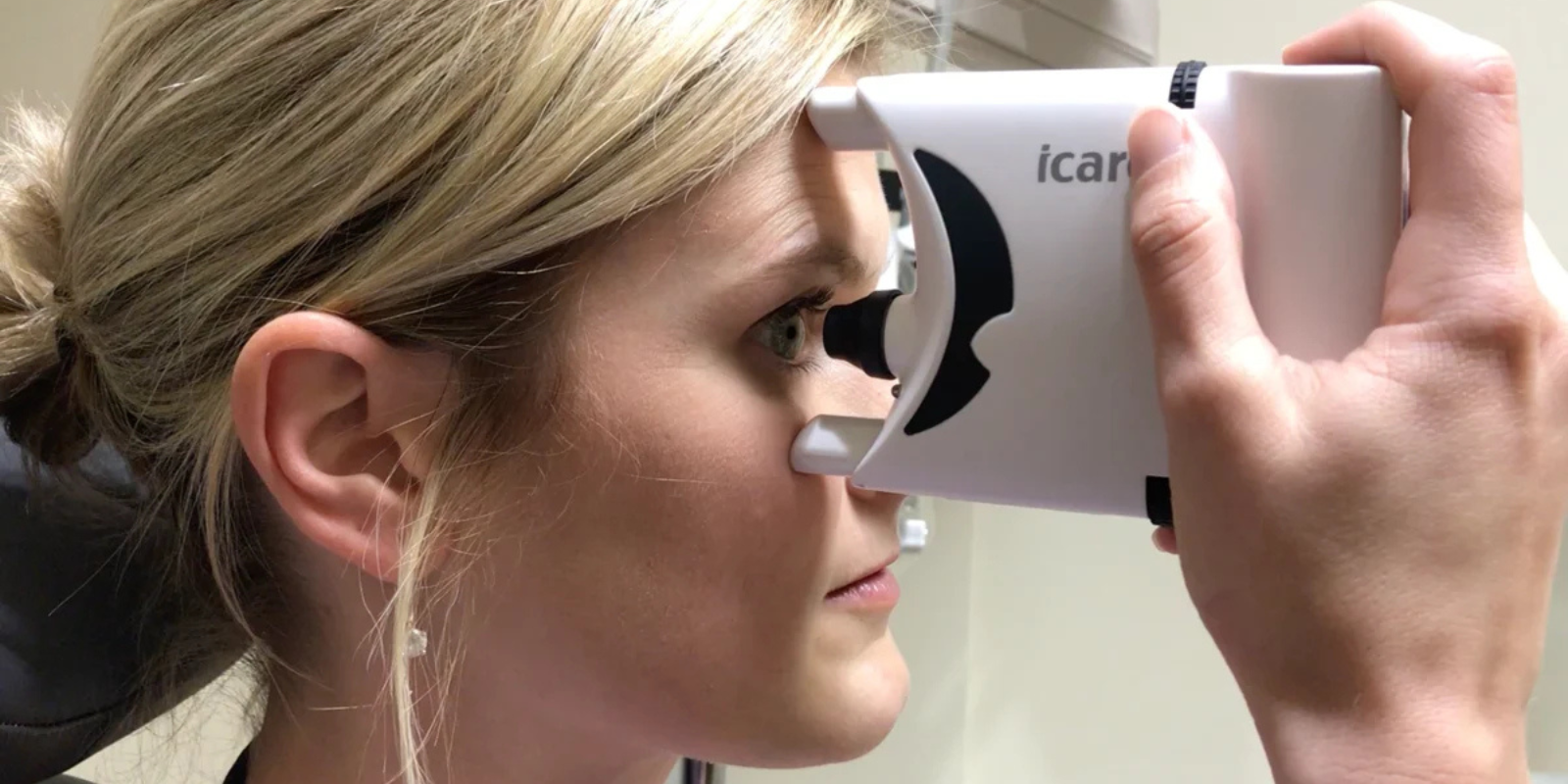
If a person is considering getting cataract surgery, ophthalmologists will conduct a variety of screening tests to assess if there are any other abnormalities that are affecting a person’s vision, such as potential retina or cornea issues.
“We measure the size and the shape of the eye, and that helps us determine the types of lens implants needed for cataract surgery,” Wildes says.
There are several different types of artificial lenses that a person can choose from, depending on how they prefer their vision to be after surgery. For example, a person may decide between choosing a lens with a prescription that restores their near vision or a lens that restores far vision. Another option is a multifocal lens that may reduce a person’s need for glasses, but it might also cause a “halo effect” associated with nighttime driving. A light-adjustable lens, on the other hand, is a monofocal lens where ophthalmologists can adjust the prescription of the lens up to three times after surgery by using ultraviolet light.
When deciding which artificial lens is best for them, a person must also consider whether they want to pay out of pocket for a premium lens, as not all lens options are covered by insurance.
If a person needs cataract surgery on both eyes, their ophthalmologist will typically operate on one eye at a time, approximately two weeks apart, to reduce visual impairment during the healing process. The surgery itself takes only about 15 minutes, and patients will typically be able to leave 30 minutes after the procedure wearing an eye patch. The day after surgery, patients have a postoperative visit with their ophthalmology team to ensure their eye is healing appropriately. Patients can expect to use eye drops multiple times a day and wear an eye patch as the eye heals.
When patients learn these details during the surgical consultation process, there are some who decide to hold off on getting surgery, Wildes explains.
“There is risk with any surgery, and we don’t want a person to go through cataract surgery and wind up having an issue where they feel their condition is worse than before,” he says. “We want this surgery to be worth it for our patients, so there is no problem with deciding to wait.”
“Cataract surgery is an incredible opportunity for patients and can be a life-changing experience,” Wildes adds. “Advances in technology have made it very safe, and new lens implant options give patients more choices than ever. It’s a privilege as a cataract surgeon to guide patients through the process and help them reach their goals for their best vision.”


.png)