Before receiving a pancreatic cancer diagnosis eight years ago – a diagnosis that resulted from persistent self-advocacy – Carolyn Degrafinried spent one awful weekend wondering if she was losing her mind.
Deep down she knew she wasn't, but for a moment it did feel that way – one of cancer’s occasional and cruel side effects. Through that terrible weekend, she had back and stomach pain so severe that she could barely move. By Monday, though, the pain was gone and never returned.
Still, she knew she hadn’t imagined that pain, and she knew something was wrong. So, she asked her primary care provider for whatever tests could help explain what was going on, and an ultrasound showed a mass on her pancreas. The initial diagnosis was that it didn’t look like cancer.
However, for several weeks after she couldn’t ignore her lingering feeling that something was off and requested more testing. This time, in April 2015, an endoscopy showed that not only was the mass on her pancreas a tumor, but it was cancerous.
A lot of things have happened since that initial, devastating news, and the path of her cancer journey has branched many times, prompting her toward often difficult choices: Accept the diagnosis or request a second opinion? Standard treatment or clinical trial? Continue with chemotherapy or commit to surgery?
At each decision point, she drew strength not only from her sense of self and self-advocacy, but from her family, her faith, and a multidisciplinary care team at the University of Colorado Cancer Center who partnered with her to create an adaptable treatment plan. In November 2022, she received the news that she showed no evidence of disease.
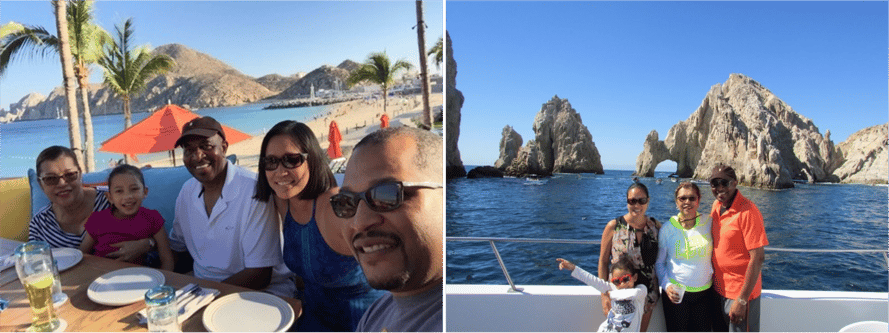
Carolyn Degrafinried enjoying time with her family.
“Carolyn is a wonderful person and a wonderful patient, and it’s been great to see her through various milestones,” says Wells Messersmith, MD, associate director of clinical services for the CU Cancer Center and division head for medical oncology in the CU School of Medicine. “She’s someone who, when I first met her in 2015, I wasn’t sure I’d see her through 2016. It’s so rewarding for me as a provider to see her today, doing so well and living her life with so much joy.”
Building a life
Ask Carolyn’s husband of 52 years, Luskey, and he’ll say that for as long as he’s known her – since high school in Somerville, Tennessee, in fact – she’s been not only someone who seeks joy, but who knows herself well enough to recognize what brings it. She is someone who trusts herself and works hard to achieve her goals.

Luskey and Carolyn Degrafinried
After she and Luskey graduated Tennessee State University in Nashville, she pursued a career in psychology and sociology, later earning a masters degree in organizational management, while Luskey entered the management track with Safeway. They moved several times for career advancement with Safeway before settling, with their young son and daughter, Alaric and Candice, in Denver in 1980.
Carolyn built her career as a teacher, transitioning to coaching new teachers with Denver Public Schools and developing and facilitating corporate education through AT&T, Avaya Technologies, and a partnership between Denver Public Schools and the University of Denver. These days, she’s mostly retired but still keeps her hand in through substitute teaching.
“I’ve always been passionate about education,” she explains, a trait also evident in her love of reading and learning. So, when she received a cancer diagnosis in April 2015, she immediately dove into research.
“I knew the standard treatment was surgery and chemotherapy, so I thought after that, and with time to recoup, that would be the end of my problem,” she recalls. “Boy, was I wrong!”
“I was just in shock”
After her endoscopy, Carolyn scheduled an appointment with Messersmith, who told her the cancer was stage 4 – meaning it had spread beyond her pancreas – and that surgery wasn’t a possibility because of the tumor’s location and the blood vessels encasing it. Surgery would be too risky because she could bleed out during the procedure and because shadows on her scans showed what might be lesions on her liver.
“Our daughter and I had to leave the room when we heard that,” Luskey remembers.
“And I was just in shock,” Carolyn adds.
It was extremely difficult news to share, Messersmith says, “and we were keeping in mind two worst-case scenarios that we try to avoid. Number one is being too aggressive – for instance, putting somebody through major surgery to take out a tumor, only to find out it had already spread and surgery was pointless, essentially. The other scenario is not being aggressive enough and foregoing a potentially curative surgery because of an image on a scan. In oncology, we often find ourselves working to find a balance between those scenarios.”
Coincidentally, before starting chemotherapy, Carolyn was chatting with another of her service providers, who told Carolyn about the excellent outcomes her father had experienced working with physicians at Memorial Sloan Kettering Cancer Center in New York City for kidney cancer. She recommended Carolyn get a second opinion there.
Learn more about getting a second opinion.
“I knew logically that was a good idea, but I also worried about mentioning it to Dr. Messersmith,” Carolyn says. “Would he be offended?”
He absolutely wasn’t. “We love second opinions in oncology,” Messersmith emphasizes. “They help me sleep at night and I always try to reassure my patients that it doesn’t hurt my feelings or undermine me. I give second opinions for other top cancer centers, too. I think we all just try to stress that we’re not in competition and that teams at various institutions are just trying to do their best for the patient.”
Looking for new treatment options
Carolyn got an appointment with Kenneth Yu, MD, at Memorial Sloan Kettering, and not only were she and Luskey able to use points by buy their plane tickets, but got a room at the Marriot next to the hospital. During their appointment, Yu said he didn’t think Carolyn’s cancer was stage 4 and he began collaborating with Messersmith on a treatment plan.
She started a FOLFIRINOX chemotherapy regimen in Colorado every three weeks, completing 13 rounds until she became allergic to one of the drugs. This was followed by targeted radiation and then five years on chemotherapy drug Capecitabine, which she took as a pill. There were side effects – hair loss over time, weight loss, dark hands and feet – “but it could have been a lot worse,” Carolyn says. “And I was alive and spending time with my family.”
During those five years, Messersmith was always on the lookout for new research or treatments that might benefit Carolyn. “One of the things that’s interesting with Carolyn is those liver lesions we initially saw on her scans disappeared after chemo. Our approach the whole time was to keep our options open. We didn’t want to be crazy aggressive or burn any bridges with chemo, but each month that goes by where the disease isn’t spreading makes us say wait a minute, maybe we should be thinking about surgery again.”
In May 2020, Messersmith contacted Carolyn with the news that surgeon Marco Del Chiaro, MD, PhD, a professor of surgical oncology in the CU School of Medicine, had newly joined the faculty and was internationally recognized for resecting tumors of the pancreas infiltrating arteries and veins.
“Dr. Messersmith brought her to my attention, and there was still a very bad vascular situation but no apparent liver lesion,” Del Chiaro says. “She had been very stable on chemo for many years and Dr. Messersmith asked if I felt comfortable trying to take the tumor out. I said, ‘It’s really risky but I think we can try.’”
Carolyn met with Del Chiaro over several appointments, discussing the pros and cons of surgery, acknowledging her hesitations and fears, praying over her choices, and eventually committed to it. On July 29, 2020, Del Chiaro performed a Whipple procedure during which he found no liver metastasis and was able to remove all of the tumor, which labs later confirmed contained no cancer cells – an indication that chemotherapy had done its job.
A new purpose for life
While her recovery was far from easy, and included a three-week hospital stay as well as several discouraging months of significant digestive issues, she leaned on her faith, her family, and her own deep reservoirs of strength. Small steps at a time, she felt more and more like herself and at an appointment in November 2022, Del Chiaro told her she has no evidence of disease.
“Praise God!” Carolyn adds.
"A lesson of Carolyn’s story is, one, be careful when you’re told a tumor isn’t resectable,” Del Chiaro says. “There may be a center where surgery is possible. And two, with multidisciplinary treatment, we’re seeing results that would have been unthinkable before, like being no evidence of disease almost eight years after a pancreatic cancer diagnosis.”
Is your pancreatic cancer resectable?
When she first received her diagnosis, all the time she may or may not have left came rushing at her, but now it’s stretching back toward the far horizon. She and Luskey – who has been with her at every appointment and every day of her hospital stay – are enjoying the sweetness of that time. They golf, spend time with their three granddaughters, enjoy their church family, and relish quiet mornings on their patio, watching the sunrise on their impeccable mountain view.
Luskey and Carolyn Degrafinried owning the dancefloor on a recent evening with family at their home.
“I’m just so grateful for my whole care team, especially Dr. Messersmith and Dr. Del Chiaro,” Carolyn says. “Because of them, I’ve been given a new lease and a new purpose for life, for which I’m eternally grateful!”





