Some battles begin before a shot is even fired, with an army building bridges and grading roads, clearing and smoothing the path to make the invading force stronger and more effective.
Some battles against cancer are following a similar strategy.
Yuwen Zhu, PhD, University of Colorado Cancer Center member and associate professor of surgery at the University of Colorado School of Medicine, is researching ways to normalize tumor vasculature — meaning the tumor’s network of blood vessels — improving pathways to the tumor so drugs and the body’s immune killer cells can better reach and attack the disease.
His groundbreaking immunotherapy research focused on tumor vascular normalization recently gained significant support from a National Institutes of Health Research Project Grant (R01). The research has the potential to treat a wide array of cancers.
The R01 grant will support the research Zhu has been conducting for more than 12 years. He and Richard Schulick, MD, MBA, director of the CU Cancer Center, along with Zhu’s former colleagues at Yale University, have a pending patent application for methods of treating a tumor by administering an agent to block a particular signaling pathway.
Zhu’s research also is supported by an American Cancer Society Research Scholar Grant, a GlaxoSmithKline grant, and a $50,000 grant from Colorado-based Wings of Hope for Pancreatic Cancer Research.
“Not directly targeting the enemy”
When he first began studying cancer immunology as a doctoral student at the Mayo Clinic College of Medicine, Zhu says, he was initially skeptical.
“I think at that time people didn’t believe cancer could be treated by immunotherapy,” he explains. “Immunotherapy is targeting the immune system. It’s not targeting the cancer directly; you’re not directly targeting the enemy. But you boost the immune system, you help it fight. At first, I wasn’t very convinced.”
However, at the first meeting with his advisor Lieping Chen, PhD, Zhu began to appreciate how immunotherapy could be used to target cancer. Chen showed him the lab’s early work to modulate cancer cells and inoculate entire tumor cell lines as cancer vaccines by targeting tumor cells to express immuno-stimulatory proteins.
“So, to me, I think this is Chinese medicine,” says Zhu, who is originally from Suzhou, China. “People talk about using a toxin against another toxin, so actually you can use a tumor to treat another tumor.”
When he began his PhD work, a lot of research was looking specifically at PD-1, a protein found on T cells that is highly expressed in many cancers and helps keep the body’s anti-cancer immune response under control. From there, and during a postdoctoral fellowship in cancer immunology at Johns Hopkins University, Zhu transitioned his research to searching for novel immune checkpoints, looking at how to prevent certain proteins, or checkpoints, from slowing or blocking the immune system’s T cells as they attack a tumor.
It is promising, important research, he says, “but only 20 to 30 patients (out of 100) can benefit from it, so how can you treat the other 70% of patients?”
Improving tumor vasculature
While continuing to research immune checkpoint inhibitors, Zhu also began looking at the complex tumor microenvironment of solid cancer, especially analyzing tumor vasculature.
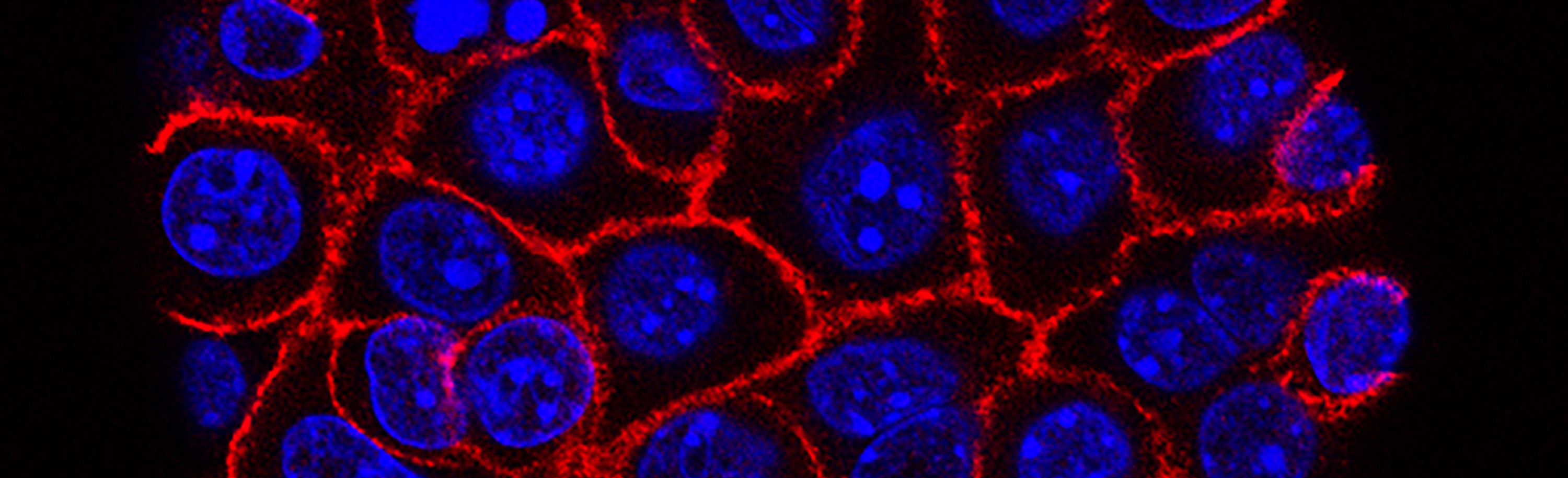
“Tumors need nutrition to grow, so they produce a lot of blood vessels to get nutrition from,” he explains. “But that vasculature is immature and irregular, kind of leaky, so basically the blood vessels are not very well-connected, not very functional in terms of the oxygen transport.
“Because they’re leaky and immature, it’s not good for immune cells to travel through to get to the tumor tissues. If we can convert the dysfunctional tumor vasculature to functional, mature vasculature, that helps drug delivery, that helps the immune response and mobilizes soldiers to those tumor sites.”
An obvious question, he says, is whether improving tumor vasculature would just make the tumor more able to get nutrition and grow faster. However, improved vasculature hasn’t led to faster tumor growth, he says.
By focusing on pancreatic cancer, which has a tumor microenvironment that is not very responsive to traditional immunotherapies, Zhu and his research partners are studying combination approaches that “reprogram” the tumor microenvironment by improving its vasculature and unleash the potential benefits of immunotherapy, including immune checkpoint inhibitors.
Fighting cancer at the tumor site
In a recently published study, Zhu and his colleagues demonstrated that insulin-like growth factor binding protein 7 (IGFBP7) interacts with its receptor CD93, and demonstrated that this interaction contributes to abnormal tumor vasculature. Blocking the CD93/IGFBP7 interaction with monoclonal antibodies, they showed, normalizes tumor vasculature, facilitates drug delivery, and sensitizes tumors to immune checkpoint therapy.
By collaborating with a startup company that has developed a CD93 antibody that can be used in humans, Zhu and Schulick are working with medical oncologists at the University of Colorado, aiming to start a first-in-human trial at the CU Cancer Center in 2022.
Zhu says he sees this research having broader applications to an array of cancers with the potential to improve already existing cancer treatments — for example, improving the delivery of chemotherapy drugs to tumors.
“One of the major reasons current immunotherapy doesn’t work — we’re talking about immune checkpoints — is because there are not many soldiers at the tumor site to fight the cancer,” he says. “The tumor vasculature is not good for them to get to the fight, so we’re helping to smooth the road.”