What are some cancer disparities facing Colorado’s Hispanic communities?
If you compare Hispanics in Colorado to Hispanics across the nation, they have a higher incidence of breast and lung cancer, and higher mortality from breast, prostate, and colorectal cancer, than Latinos elsewhere. But if you compare non-Hispanic whites in Colorado to non-Hispanic whites around the country, those in Colorado have significantly lower incidence and mortality rates of these cancers.
Are there parts of the state where disparities are more pronounced than others?
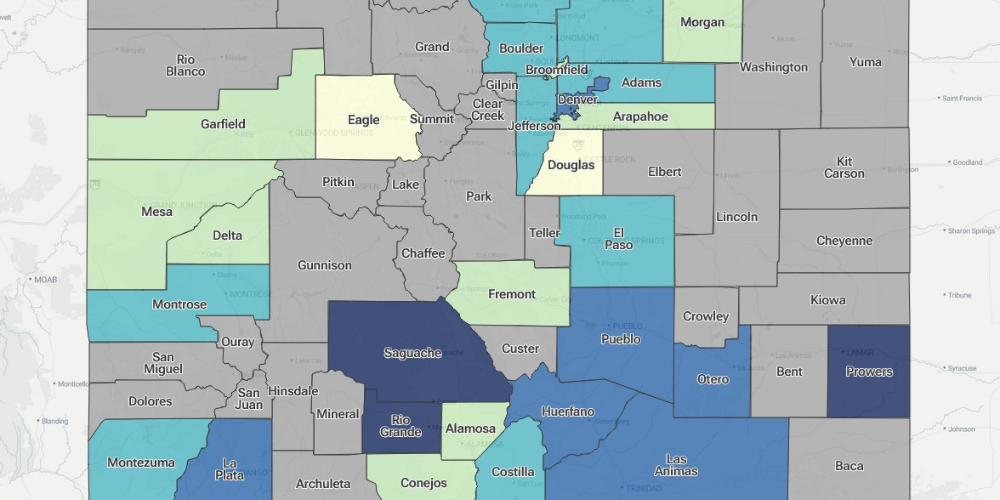
Overall, the southeastern counties of Colorado, bordering New Mexico, tend to have higher disparities, and not just for cancer. A lot of Hispanic people live in these counties. These areas have a shortage of access to things like radiation oncology, medical oncology, and surgical oncology. Pueblo and Colorado Springs are the closest large cities to these areas, but people have to travel to access care.
What are some social determinants of health and risk factors that may figure into cancer disparities among Hispanic people?
These include poverty, housing, food insecurity, lack of local access to health care, lack of physical activity, and environmental factors. Obesity is high in some communities, and the lack of access to healthy foods contributes to that.
Also, smoking rates are higher in Hispanic populations compared to non-Hispanic whites, particularly among working-class males. Smoking rates are going down statewide, but among Hispanics they’re slowly increasing. Type 2 diabetes, which is a risk factor for cancer, is higher among Hispanics.
Insurance is a factor, too. Many people in Hispanic communities are on Medicaid, and some are completely uninsured because of a lack of documentation. Southeast Colorado has a high migrant population working in fields seasonally. They come in and out of the country, and many of them don’t have access to insurance or medical care.
And rates of early detection of cancer – being up to date with screenings – tend to be lower among Hispanics for breast, cervical, and colorectal cancer. Often they don’t get their mammogram or their colonoscopy or their Pap smear.
Are there cultural or educational factors that come into play?
Among some, not all, Hispanics, there may be a reluctance to talk about cancer, perhaps driven by socioeconomic factors and a lack of awareness. There’s a sense of, “Don’t be talking about those negative things or you may be asking for them.” Or, “Why would I do a mammogram? It’s going to find something wrong.”
We do a segment on Spanish radio each month, on “Hablemos Hoy,” that reaches the majority of the area’s Spanish-speaking population. We tell people, “These are things you’ve got to talk about. It’s better to prevent it now than to be sorry about it later.”
What are some other ways that the CU Cancer Center and COE are working to address these disparities?
Our charge is to bring the mission of the CU Cancer Center to communities, and particularly to underserved, disadvantaged communities. And much of what we do is education. As I mentioned, on Spanish radio, every month we’re educating people and taking questions about cancer.
We do a lot of awareness programs in communities. We talk about the importance of early detection and prevention, about diet, about not smoking, drinking, and so on. We also offer the 2Morrow smoking-cessation app free to anyone in Colorado.
As far as cancer screening goes, the CU Cancer Center is distributing free colorectal cancer screening kits that can be used at home, targeting uninsured people across Colorado with lower rates of screening. These are fecal immunochemical tests (FIT) kits. We are distributing those to individuals who may not have a medical home. We go into communities through health fairs, county fairs, other events, libraries – wherever we can reach people.
We also distribute free radon kits for people to be informed about whether radon is high in their homes. Some people don’t have a radon mitigation system in their home or apartment. So we advise people to test their home, and if they need mitigation and can’t afford it, we can help connect them to resources.
We help navigate low-income people to other kinds of screening as well as to care. And we try to navigate them into clinical trials if they qualify.
Awareness goes a long way. In the Hispanic community, because family is so important, we encourage people to talk to their family members about early cancer detection, about diet, about smoking and radon and environmental risks.