Abbey Lara, MD, suspects she first encountered a patient sick with COVID-19 in February 2020, though she has no way of knowing for sure. At the time, working in the medical intensive care unit in the University of Colorado Hospital, the patient just seemed like a unique case — sick with acute respiratory distress syndrome but reporting feeling fine.
“He wasn’t behaving in a way that I would have expected. He was able to talk in full sentences and refused being intubated because he felt fine, even though he was on the maximal amount of oxygen we are able to provide outside of intubation. It was unusual,” says Lara, a pulmonologist and critical care physician.
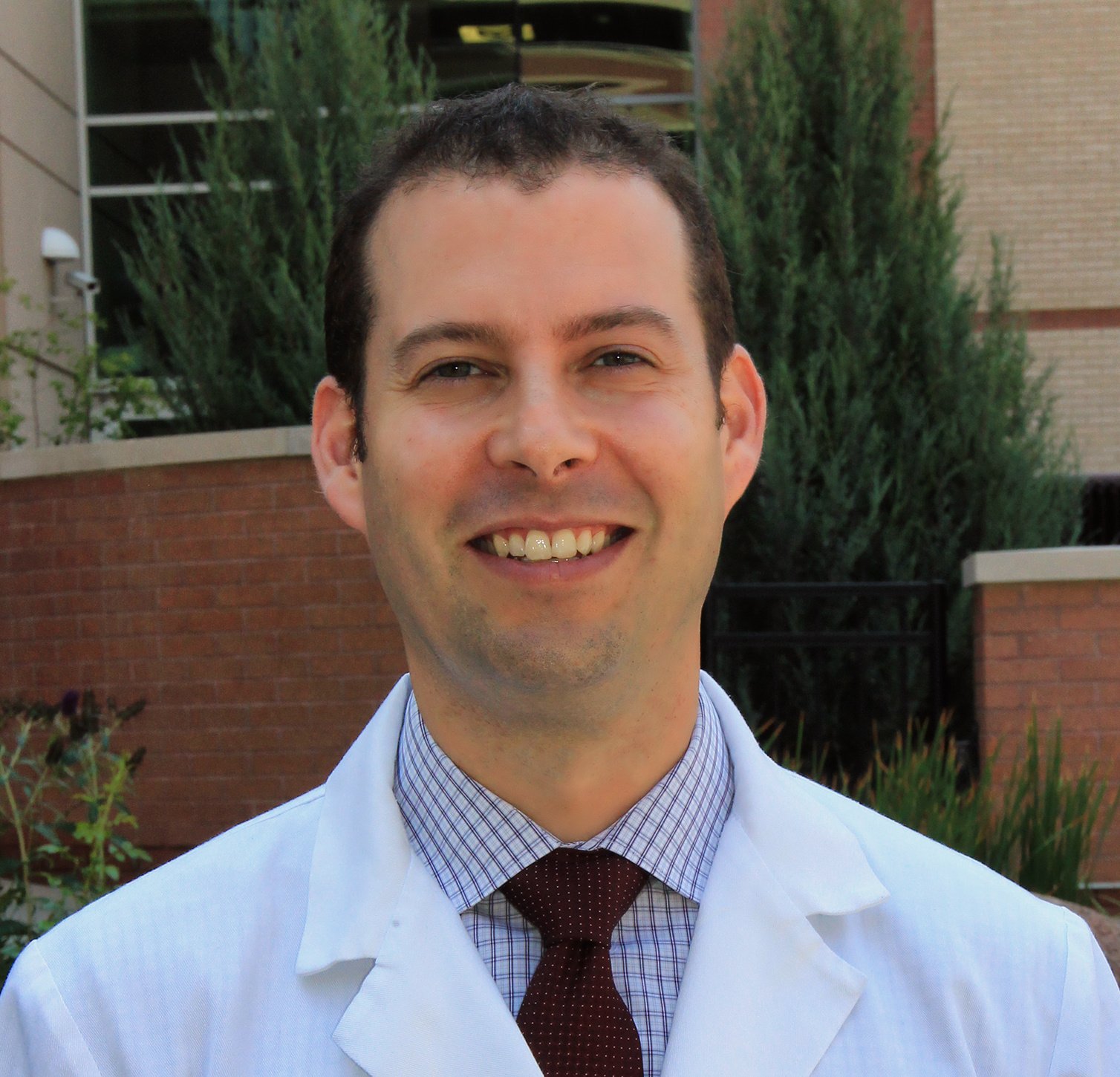
Across the world, infectious diseases physician Steven Johnson, MD, was in Zimbabwe as part of the CU Department of Medicine’s Colorado-Zimbabwe International Exchange program. He recalls speaking with colleagues about the rumblings they’d heard of COVID-19, wondering if it could be similar to other diseases like the original severe acute respiratory syndrome (SARS).
He returned to Colorado on March 1, just weeks before, as primary care physician Rob Doolan, MD, puts it, “the world stopped.”
Hospitalist Jonathan Pell, MD, was on a spring break vacation with his wife and two children when he received a notification that his children’s school would not be resuming in person.
“When I came back to work, we were already having a disaster response team of hospitalists come together to plan how to care for patients and track information in electronic health records,” he says.
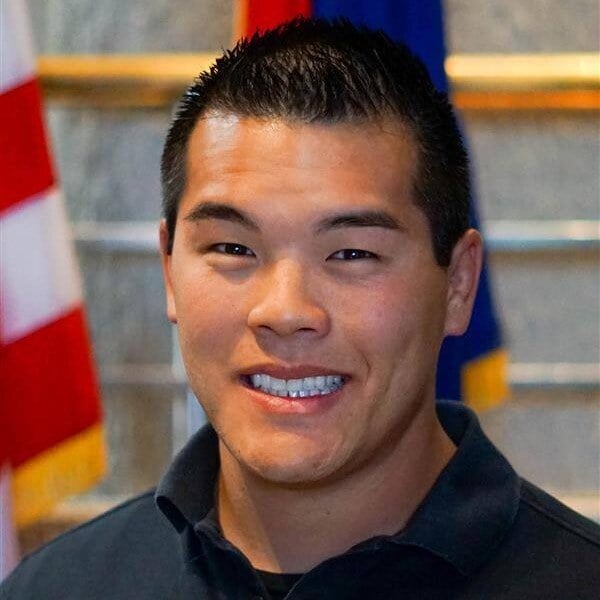
Nicholas Vuong, NP, MSN, typically avoids talking about his experience working as a nurse practitioner in the ICU during the pandemic. He remembers the many patients whose lives were lost, and the family members he had to tell the devastating news to.
“My mind has tried to bury it,” he says. “One of the hardest parts about COVID-19 was the family conversations. We’d talk about how sick their loved one was, and for many, we had to tell them that their loved one was dying.”
In a time of uncertainty and tragedy for many, these clinicians and their colleagues at the CU Anschutz Medical Campus banded together, working diligently to provide the best care possible and save lives. It has been five years since the COVID-19 pandemic was declared, but its lingering effects, positive and negative, still show up, whether it’s through innovating better methods of delivering care, building trust with patients, dealing with secondary trauma, or collaborating with — and leaning on — other clinicians for support.
The early days
Colorado’s first official case of COVID-19 was reported on March 5, 2020, and by March 11, the World Health Organization declared COVID-19 a pandemic. Colorado reported its first COVID-19 death on March 13 — one of 4,315 reported COVID-19 deaths in the state that year.
Lara still has a screenshot of a mobile emergency alert from Denver on March 24 announcing a stay-at-home order for residents and businesses. Soon after, Governor Jared Polis put the entire state on lockdown, effective March 26.

A screenshot from when Abbey Lara, MD, received a stay at home order on March 24, 2020. Image courtesy of Lara.
By the last week of March, the critical care annex of the University of Colorado Hospital was slated to become the COVID-19 unit, Vuong recalls.
“I remember that first day we started with maybe two or three patients. By the end of the week, we had 20 patients,” says Vuong, an instructor in the Division of Pulmonary Sciences and Critical Care Medicine. “It was the same kind of intensity as there normally is in the ICU, but there was also a lot of uncertainty. As time went on, it was more isolating because you were confined to the area. It was very quiet, because there were no family members in the units.”
Pell, an associate professor in the Division of Hospital Medicine and the senior medical director of informatics for UCHealth inpatient services, worked to care for hospitalized patients and create electronic health record tools to aid other clinicians.
“At the hospital, you never really knew what the next day was going to bring,” Pell says, explaining that clinicians spoke daily to talk through their experiences and compare notes on how to improve care. “We were learning stuff on the fly. The standard of care was essentially evolving week-to-week.”
One bright spot at UCHealth, Lara notes, is that unlike many other hospitals and academic medical centers across the country, the hospital was more prepared for the pandemic in terms of personal protective equipment (PPE) because leaders had previously stored materials like N95 respirator masks amid concerns about the spread of Ebola roughly a decade before. As she focused on providing care to scared patients, it was comforting to know she would not run out of PPE.

Abbey Lara, MD, wearing personal protective equipment while working in the hospital during the COVID-19 pandemic. Image courtesy of Lara.
Outside of the inpatient units, Doolan, a Division of General Internal Medicine associate professor of clinical practice, was only six months into his new role as the associate division head for clinical affairs — overseeing about 60 clinicians and 60 medical residents across five outpatient clinics — when COVID-19 struck.
“We had a period where everything was shut down, and then we quickly pivoted to virtual sessions,” Doolan says. “We essentially went from zero telehealth visits to immediately trying to figure out how to see all of our basic visits with telehealth.”
And on a national level, Johnson, a professor of infectious diseases and renowned expert in HIV/AIDS, joined the National Institutes of Health COVID-19 Treatment Guidelines Panel, helping create and update guidelines for health care providers across the country on how to treat COVID-19.
“I saw similarities between HIV and COVID-19 in terms of it being a new disease with high lethality, and a need to rapidly develop information, medications, and a vaccine,” Johnson says. “It was a very rewarding time, but it was also a time of anxiety, as there were a lot of critically ill people and deaths.”

The National Institutes of Health COVID-19 Treatment Guidelines Panel on Dec. 16, 2022. Steven Johnson, MD, is standing in the second row from the back, second person from the far right. Image courtesy of Johnson.
Remembering lives lost
It brings tears to the eyes of several clinicians as they remember the patients they cared for during the pandemic and the conversations they had with patients’ loved ones.
For Lara, she carries the memories of three people, in particular. A woman in the ICU who kept saying how scared she was when Lara talked with her about putting her on life support. A colleague who died in December 2020 due to COVID-19, and the small candle enclosed in a glass that Lara and her colleagues place in the ICU to remember him every December. And a male patient who Lara cared for during her first week in the COVID-19 ICU, and his family’s desperation to see him as he approached his final moments.
“He was doing very poorly, and we called his family to let them know that we were worried he was about to have a cardiac arrest. His wife of more than 40 years kept begging, ‘Let me see my husband,’” Lara recalls. “We were able to get permission for her to put on PPE so she could see him. She was so grateful for those less than five minutes before he died.”
From the countless patients Vuong helped care for in the COVID-19 ICU, one that really sticks in his mind is a 25-year-old man and his mother. Soon after transporting the man from the emergency room to the ICU, his vital signs started crashing and he began coding. Vuong and another physician took turns doing CPR, and another nurse called his mom to come up to the room. But after 45 minutes, the man was pronounced dead.
“I got out of the room, drenched in sweat, and I saw his mom walking into the unit. I had to tell her, ‘We tried everything we could, but we couldn’t save your son,’” Vuong says. “She fell to the ground and let out a piercing scream. It was terrible.”
The survivors
It’s not only the lives lost that stay with clinicians — it’s also the lives saved. Johnson still gets choked up when he thinks of a woman who survived COVID-19 and the stark difference between the first and last time he saw her.
“We did telehealth visits with people who had recovered, and one of my visits was with this woman who I only remembered as being face down, unconscious, and on a ventilator in the hospital,” Johnson says. “On the call, she was happy and thankful. She had these bright red plastic glasses on. It made me emotional, because during COVID-19, there was an extraordinary amount of death. But there were also patients who seemed like they wouldn’t survive, yet they did.”
For Pell, he remembers a man who narrowly survived. The patient had a high body mass index, was a previous smoker, and had already survived brain cancer. Pell worked diligently to provide care so that the man would not have to go to the ICU, because he believed that if the man was intubated, he would have a less than 25% chance of surviving.
“He was in the hospital right when we found out that steroids were helping COVID-19 patients, so he was one of the first patients of ours who got high-dose steroids. He never went to the ICU, survived the hospitalization, and did well afterward,” Pell says. “He’d told me that he had this old, expensive bottle of scotch that he drank from when he survived his brain cancer. During COVID-19, I remember him saying, ‘If I get out of this hospital, I’m gonna get another pour of that scotch bottle.’”

Abbey Lara, MD, (far left) and other clinicians in the COVID-19 intensive care unit created "life links" to highlight when a patient left the COVID-19 ICU and transferred to a floor in the hospital. Image courtesy of Lara.
A rise in distrust
As the pandemic went on, and lockdowns were extended, clinicians noticed a shift in the attitude of some people toward medical providers.
In the beginning, there was an outpouring of community support. Doolan remembers hearing the ringing of bells and cheers from his neighbors each day at 5 p.m. in recognition of health care workers.
“That didn’t last very long. But when it happened, it was meaningful,” he says.
Pell says he noticed a change around the summer of 2020, and especially during the fall and winter as COVID-19 vaccines started becoming available.
“We had patients throwing coffee cups at nurses for offering vaccines, accusing the nurses of trying to kill them,” he says.
Because of the strict COVID-19 regulations during the pandemic, many people were unable to be with their loved ones who had been hospitalized, instead having to rely on conversations with clinicians like Vuong. One of the difficulties was when family members struggled to understand how poorly their loved one was doing.
“You’d tell them that the patient was dying, and the family member would say, ‘But are they?’ People also started reading these things online that said COVID-19 isn’t real, so some thought we were hiding things from them about their loved ones,” he says. “It’s hard when they can’t see the patient themselves.”
Information polarization still lingers
Addressing misinformation, about vaccines in particular, was another challenge each clinician faced. Patients were receiving conflicting information from health institutions, the media, and politicians, and clinicians were left to address questions and deal with the mixed reactions from patients. As a primary care physician and clinical leader, it’s an issue that Doolan still sees.
“I think the biggest consequence of that period was the constant push of a lack of trust in science and what we do. The misinformation that was put out caused ongoing harm, and I think patients have a much bigger mistrust in the health care system as a whole than they did previously, particularly about vaccines,” Doolan says. “What are the consequences of that? Now, we’re seeing measles outbreaks. It’s a huge problem.”
Being a member of the national guidelines committee for COVID-19, Johnson had the advantage of talking firsthand with investigators who conducted research into different treatments for COVID-19.
“There was a lot of drama about which therapies were effective and how they should be used. When you came out against a certain medication, like hydroxychloroquine, you’d get a flurry of messages that were very abusive from some people, accusing you of trying to kill people,” Johnson says.
“One of the lessons from the pandemic was that the relationship you have with patients matters,” he adds, emphasizing the importance of patients knowing they can trust their clinicians. “The downside of social media is that people have access to large volumes of inaccurate data. Since COVID-19, and even before then, I’ve had to help people handle misinformation and provide them scientific, evidence-based information that they can act on.”

Steven Johnson, MD, received the COVID-19 vaccine for the first time on December 19, 2020. Image courtesy of Johnson.
The nuance of COVID-19 and how it has evolved over the past five years is also sometimes lost in the conversation, Pell says, explaining that the disease now generally has less severe symptoms mostly thanks to the vaccines, therapies, and interventions offered early on in the pandemic.
Johnson adds: “We now have a population that has acquired immunity, in part from COVID-19 infection and in part from vaccines, so it’s safer if people are exposed to COVID-19 today compared to 2020. Because the majority of the population now has a stronger immune system for this virus, I wonder if we conducted the same trials of therapies we did in 2020, would we still have the same results?”
Relying on each other
Although the pandemic had many lows, there were also some positives that came from it — chief among them was the collaboration among health care workers to innovate better ways to treat patients.
Pell, for instance, says he and other hospitalists felt more valued and involved as they worked alongside other clinicians to treat COVID-19 patients.
Lara agrees, saying: “It was all hands on deck. People came together. People did jobs that they might not have been hired to do. There was such a sense of teamwork and focus on providing the best care possible for the patient.”
It was this sense of teamwork that helped create a supportive community for these clinicians, which was especially needed as other health care workers decided to leave the field due to burnout. Doolan explains there was a big resignation phase that created issues for the clinics he oversees, saying, “There was a lot of flux that was extremely difficult to get through. We’ve spent so much effort to restabilize our clinical workforce.”
Ultimately, what kept each of these clinicians in their field was a sense that their work was not only needed, but it was also deeply valued by their colleagues, supervisors, and by many of their patients at the CU Anschutz Medical Campus.
The next five years
With the lessons of the COVID-19 pandemic in mind, as these clinicians look ahead to the next five years, each underscore the need for continued investment in research and establishing the infrastructure needed to respond to health crises.
“Emergency preparedness is important. UCHealth was ahead of the game compared to the rest of the country. We never ran out of PPE, and we never ran out of ventilators,” Pell says.
Lara says the CU School of Medicine, University of Colorado Hospital, and UCHealth leaders “did an exceptional job at standing up the infrastructure and operations to support the mission of an academic medical center,” adding that she also appreciated the transparent and frequent communication delivered by health leaders and organizations.
“My hope is that local leaders don’t forget how to do that. Nationally, we must continue to recognize that scientific discovery is truly how we impact clinical care,” she says.

Abbey Lara, MD, with her colleagues in the medical intensive care unit. She says they are like family to her. Image courtesy of Lara.
Vuong, Doolan, and Johnson share similar sentiments, saying they want to see health leaders prioritize preventative care and investment in scientific research.
“We have to prioritize preparing for the next pandemic — which involves having a functional public health system on a state and national level, having the right kind of testing, and having case finding so the next pandemic can be detected as soon as possible,” Johnson says.
Vuong adds: “Over the years, there are hundreds of things that could have become a pandemic but were able to be stopped because of our protocols, research, and vaccines. No one should have to deal with something like this pandemic again.”