Can a change in diet make it easier for women to get pregnant? Researchers at CU Anschutz say simple dietary changes, even for short durations, may help.
Irene Schauer, MD, PhD, who studies insulin resistance and its impact on the cardiovascular system, and Nanette Santoro, MD, who studies infertility and obesity, joined together to find whether insulin resistance contributed to decreased fertility.
What they found may someday make a difference in fertility issues, which impacts approximately 1 in 10 women of childbearing age in the United States.
Insulin resistance leads to poor cardiovascular outcomes
Obesity and diabetes are risk factors that contribute to cardiovascular disease – a main cause of death in the United States and worldwide. Insulin resistance is a complex condition marked by both genetic and lifestyle factors and can lead to diabetes.
“With obesity, we know there is usually insulin resistance,” said Schauer, clinical professor of medicine in the Division of Endocrinology, Metabolism and Diabetes at CU Anschutz School of Medicine. “But how that plays into the vascular function is not totally clear.”
A few years ago, Schauer designed a study to temporarily induce insulin resistance in otherwise healthy people to study the impact on vascular function and exercise. She was able to raise fatty acid levels through a six-hour infusion of lipids, making the healthy participants more insulin resistant.
Santoro, professor and E. Stewart Taylor Chair in the Division of Reproductive Endocrinology and Infertility, studies repro-metabolic syndrome – a term used to describe women with obesity who have trouble getting pregnant. After seeing how Schauer’s team induced insulin resistance through lipid infusion, she reached out to see if their data might shed light on whether insulin resistance might contribute to decreased fertility.
Using blood samples from Schauer’s study, the researchers found preliminary data showing that the signaling between the pituitary gland and ovaries was disrupted when fatty acid and insulin were both high, and insulin resistance was induced.
“The results were encouraging enough that we then did a lipid infusion study as a collaboration,” Schauer said. “We found that indeed, in lean women with normal menstrual cycles, if you infuse lipids and insulin and cause insulin resistance, that interferes acutely with the pituitary-to-ovary signaling.”
Can diet changes improve fertility?
Specifically, the conditions that induced insulin resistance also interfered with the luteinizing hormone released from the pituitary, which triggers ovulation and the follicle-stimulating hormone that stimulates the development of eggs.
Armed with this knowledge, the researchers then developed a study to explore whether a temporary high fat diet, designed to not cause weight gain, could also induce insulin resistance in healthy women. They reasoned if a high-fat diet can make someone insulin resistant, the reverse may also be true, meaning a temporary low-fat diet may help to restore the signaling pathway in women with obesity who are experiencing decreased fertility.
“Obviously, weight loss for these women would be a solution, but we all know that weight loss is not easy. So we started with the premise of inducing insulin resistance in lean women by giving them a high-fat diet, to explore the potentials of a therapeutic path,” Schauer said.
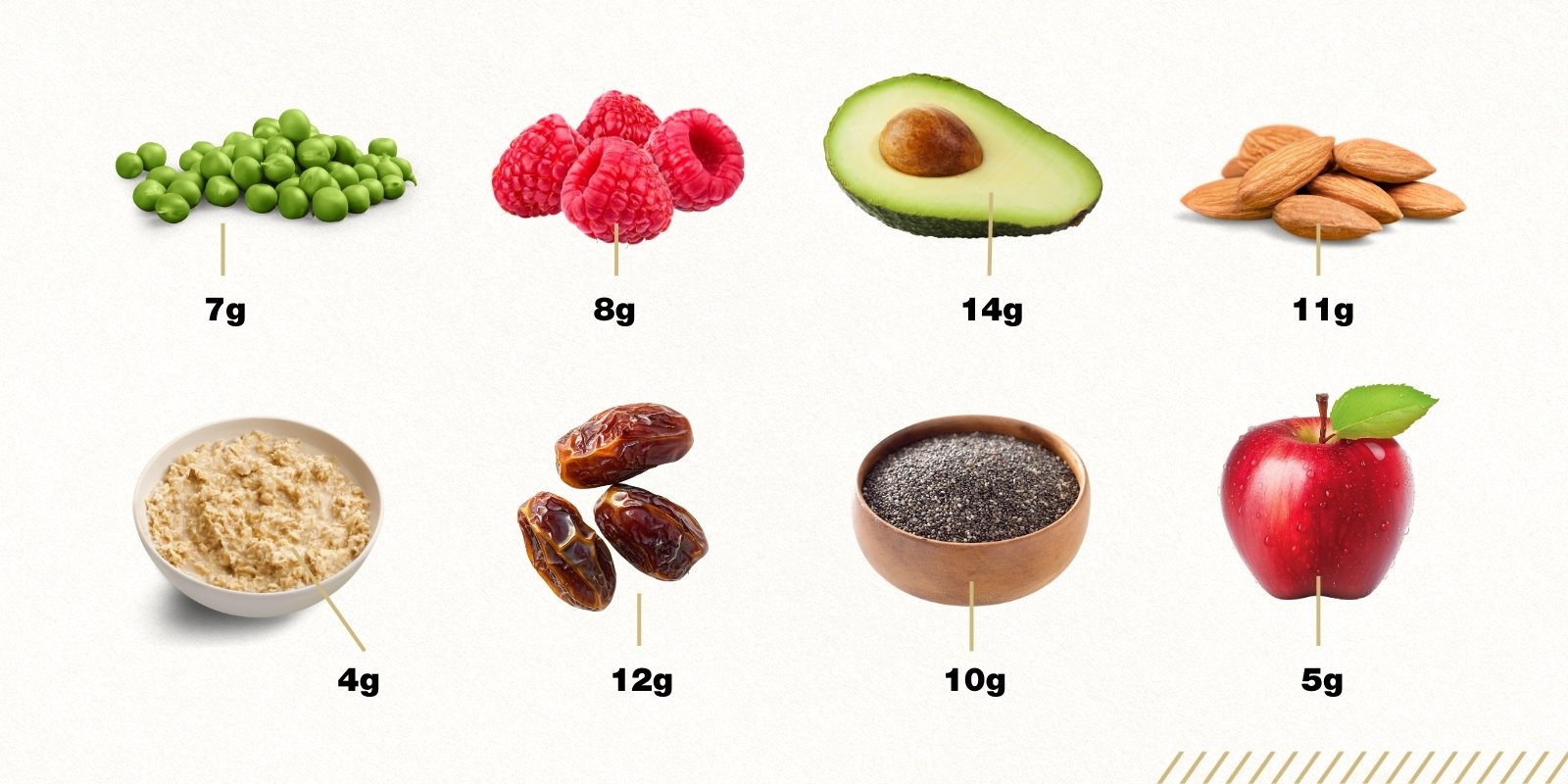
To learn whether diet composition by itself could be a factor that impaired fertility in obesity, the researchers placed 18 lean, healthy women on a specific diet. The women had normal menstrual cycles and were not trying to get pregnant. The prescribed diet was eucaloric, meaning they consumed just enough calories to maintain their current weight. The diet was high in fat (48% of calories) and emphasized healthy fats, such as those found in avocados, nuts and other foods high in omega-3 and omega-6 fatty acids. They provided the women with all the food consumed during the four-week intervention.
The researchers found that the high-fat diet did increase insulin resistance in the women. Results showed that the signaling from the pituitary gland to the ovaries was impaired, similar to what was seen in women with obesity and in the women from Schauer’s initial lipid-infusion study.
Interestingly, while all the women’s numbers moved in the same direction, the amount of induced insulin resistance didn’t necessarily correlate with the degree of impaired signaling, which Schauer said might be due to the small size of the study.
She believes these findings about insulin resistance and high-fat diets could have implications for obese women who struggle with fertility.
“The study suggests that women with obesity may be able to improve their fertility just by going on a low-fat diet, without needing to lose a significant amount of weight. A low-fat diet may be enough to improve pituitary signaling and ovarian function,” Schauer said.
Santoro is currently working to expand this study by providing a low-fat diet to women with obesity.
Diet changes impact the microbiome
During the study, the researchers took samples of the women’s gut microbiome, because some evidence suggests gut health may play a role in obesity, poor fertility and impaired pituitary-to-ovary signaling. People with obesity are thought to have a less-diverse gut microbiome – a “dogma” that Schauer said this study may challenge.
“What we found in the women in this study was that after eating a high-fat diet for four weeks, the women had greater diversity in their microbiome by multiple different measures,” she said.
Schauer said the findings were a surprise, so they consulted the nutrition core to get more information about what the participants ate.
“The diet was designed to increase ‘healthier’ fats, such as monounsaturated and polyunsaturated, as opposed to foods high in trans fats that are prevalent in Western diets,” Schauer said. While they specified that the diet be high in fat, they hadn’t specified anything about fiber, which is associated with a more diverse microbiome.
“When we looked back, we saw that the diet they designed was higher in fiber than the typical Western diet,” Schauer said. “So while the high-fat diet was unhealthy in some ways, it was potentially higher in fiber than they were eating before. And that turned out to have some potential benefits in terms of their microbiome diversity.”
She recently presented findings from the high-fat diet study at a conference where she learned more about the complicated nature of the microbiome.
“To go into fertility was a side road for me, but it kindled an interest about how the microbiome correlates with risk factors for cardiovascular disease,” Schauer said. “My takeaway is that there may be some individual variation, but it’s clear that to some degree, fiber and moderate levels of healthy fats are part of a healthy diet. We certainly have good evidence for the importance of a healthy diet for good cardiovascular, reproductive and metabolic health.”
.png)