Eye drops can be a double-edged sword, says Richard Davidson, MD, professor of ophthalmology at the University of Colorado School of Medicine.
They can be helpful in treating serious ocular conditions, like managing intraocular pressure (IOP) in glaucoma patients or lubricating dry eyes, but they also present difficulties for some patients.
“Patients don’t always like using eye drops, and doctors don’t always like prescribing them,” says Davidson, who has an endowed chair in eye care innovation. “We’re trying our best to alleviate the need for drops as much as possible, either because they can be irritating to the ocular surface or because there are compliance issues.”
READ MORE: How CU ophthalmologists are working to improve eye drop compliance
As a result, the world of ophthalmology is seeing a number of innovations and new uses for eye drops. While some newly developed devices aim to side-step the need for eye drops completely, physicians are also gaining access to drops that may have fewer symptoms and make taking the medication easier for many patients.
“There’s a lot of science that goes into these tiny bottles,” Davidson says. “It can become pretty complex, depending on what we need the eye drop to do.”
Evolving formulas make for better treatment
Preservatives used in eye drops help prevent bacteria and fungi that can cause infection, but they’re also harsh on the ocular surface. In some instances, like glaucoma, patients may need medication to control the condition but don’t experience any noticeable symptoms, including irritation and discomfort, until they start using eye drops due to the cumulative effect of placing preserved drops in the eye over weeks, months and years.
“There’s a ton of work right now to reduce the amount of benzalkonium chloride, a common preservative in drops,” Davidson says. “Researchers are looking to make these medications more self-preserved, which could cut down on that irritated feeling many people get.”
Some drug companies are also looking at the way the medication is packaged in the eye drop container.
“You may have the same medication and the same active ingredient, but this newer technology is allowing the medication to get into the eye more rapidly,” Davidson explains. “With this comes less irritation on the ocular surface, and the molecules have better penetration.”
Looking beyond the bottle
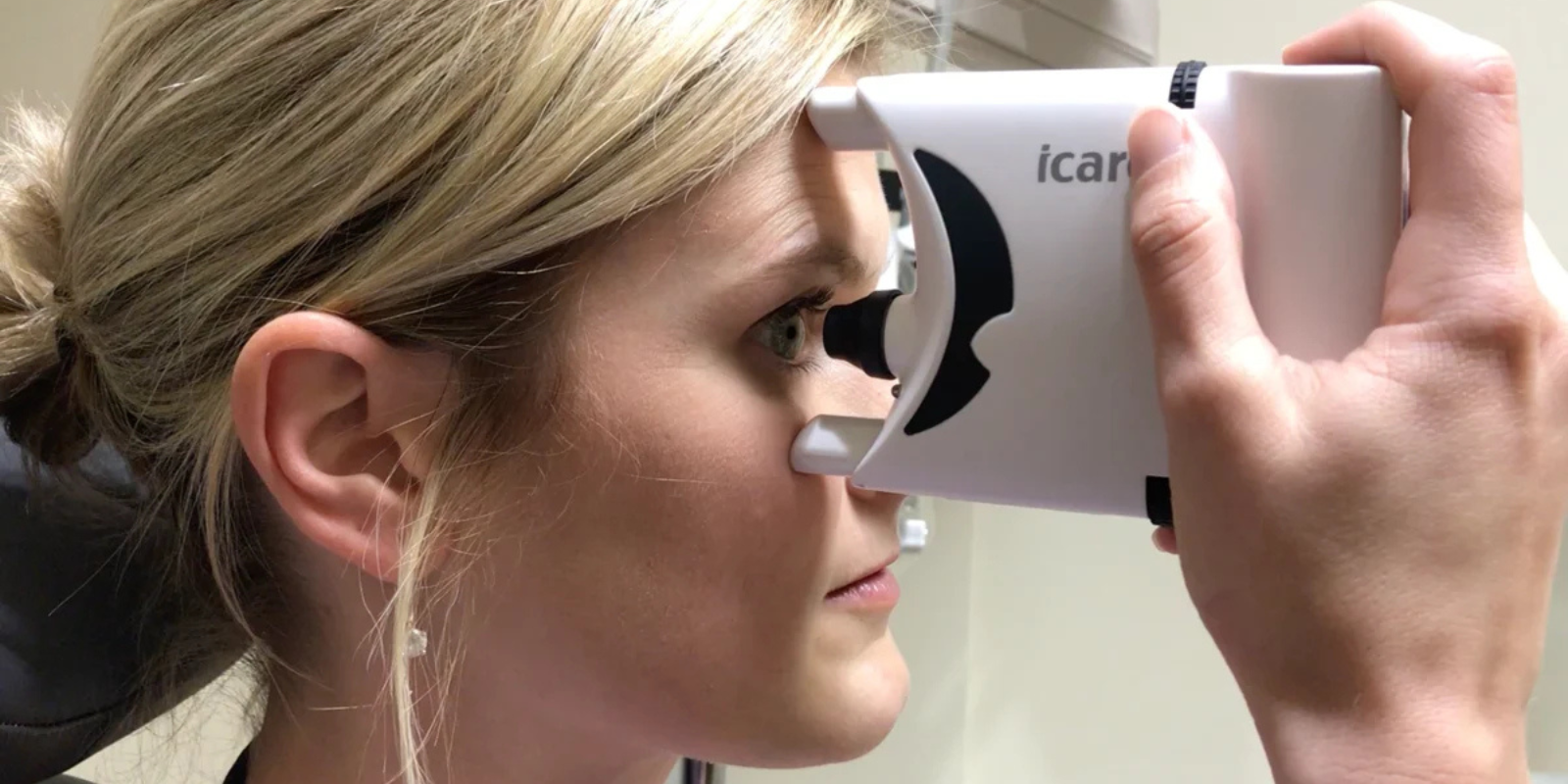
In other instances, ophthalmologists are looking for ways to bypass drops altogether. New technologies that implant into the eye are showing promise in delivering medication consistently without the need for drops.
“The current trajectory is trying to get rid of drops as much as possible,” Davidson says.
However, doing so can be complex, and options are limited to treatments that can be administered directly to the eye. The eye is physiologically walled off from the rest of the body, so it’s not a simple feat to develop drugs for ocular conditions in a tablet or pill form that could be taken orally.
“They just don’t penetrate the eye like we need them to,” Davidson says. “We will never get rid of drops altogether. They’re used in so many different ways. That why there’s so much focus on making the drops we have better.”
READ MORE: Why ophthalmologists turn to eye drops to treat ocular conditions
New uses in ophthalmology
Despite existing challenges, eye drops are still proving to be helpful in new ways.
In 2021, the Food and Drug Administration (FDA) approved eye drops that treat presbyopia, an age-related condition causing blurry vision that affects approximately 128 million people in the U.S.
The drops constrict the pupil, which can extend range of vision.
“I have some patients who really like it,” Davidson says. “Other patients find that a constricted pupil tends to dim their peripheral vision. If the pupil doesn’t dilate, it’s not letting light in.”
Risks for using the drops include the potential for retinal tears and detachment.
Also related to vision, researchers are now looking at the use of atropine eye drops to treat myopia, particularly in children, but there isn’t a treatment approved by the FDA yet.
“Right now is an exciting time in ophthalmology. We’re looking at many ways to make treatment for ocular conditions better and finding success in making these drops simpler and less bothersome for patients,” Davidson says.